Spatial Patterns of LRTI among Children in Lahor
Shaista Manaf1, Dr. Ibtisam Butt2
1,2 Department of Geography, University of the Punjab, Lahore, Pakistan
Corresponding author: binashaista9@gmail.com
Citation | Manaf. S, Butt. I, “Spatial Patterns of LRTI among Children in Lahore”. International Journal of Innovations in Science and Technology, Vol 4, Issue 1, pp: 51-64, 2022.
Received | Dec 01, 2021; Revised | Dec 12, 2021 Accepted | Dec 20, 2021; Published | Jan 28, 2022.
________________________________________________________________________
Lower Respiratory Tract Infection (LRTI) is the leading global cause of morbidity and mortality in children of 1 month in developing countries. The aim of this research was to examine the spatial patterns of children under LRTI in Lahore, Pakistan. The records of all patients of LRTIs among children <5 years, admitted in the four different public sector hospitals of Lahore from 2017-2021 were analyzed. The collected data was processed and analyzed in SPSS 22.0 for the chi-square test (P<0.0.5), Multiple linear regression and ANOVA were calculated to assess the association of these variables. Town-wise distribution of diseases was mapped in ArcGIS 10.5. There were 2,609 pediatrics patients admitted and major cases in the year 2021. All the patients were distributed in four age groups, <2m, 2-12m, 13-24m, 25-60m. The most common diagnosis was Bronchopneumonia with (77.50%), Bronchiolitis (11.84%), Pneumonia (6.86%), and Bronchitis (3.79%). A significant increasing trend was found in Bronchopneumonia. In town-wise analysis, out of 2,609 patients, 977 patients were observed in Allama Iqbal Town. The peak season of the disease was seen in winter Dec-Feb. LRTI is a leading cause of childhood hospitalization in Lahore, Pakistan. These results may guide health authorities to determine where and when to effectively allocate resources for the prevention and control of LRTI.
Keywords: LRTI; ArcGIS 10.5; seasonality; Bronchopneumonia; children; chi-square Test and ANOVA.
INTRODUCTION
Health geography can provide a spatial understanding of a population's health distribution of disease in an area [1]. The researches which bring geography and medicine together have been followed since long ago. The initial studies tracked the diffusion of infectious disease, but the research that highlights spatial variances in several health-related weaknesses is not new and continues to prevail today.
A healthy child makes an energetic generation. There is a close association among unhealthy children to a weakened future of the world [2]. Respiratory infections are a foremost cause of morbidity and mortality in children under five years of age globally [3, 4, 5, 6]. Approximately, 6.6 million children less than 5 years of age die each year in the world; 95% of them are in low-income countries [7] and one third of the total deaths is due to LRTI [8]. WHO assessed the rate of respiratory tract infections in 2010, according to estimations four and a half million deaths due to respiratory tract infections among children every year [8, 9, 10, 11]. In South Asia, 48 of every 1000 children die before the age of five. Pakistan is presently placed as the sixth most populated country with a population of 199 million. It is estimated that about 20% to 30% of deaths of children under 5 years of age are because of respiratory infections in Pakistan [12].
Lower respiratory infections caused 652, 572 deaths in children younger than 5 years worldwide in 2016. Particularly, Acute Lower Respiratory Infection (ALRI) in the form of pneumonia is recognized as the single largest cause of childhood death globally accounting for 16% of the overall deaths in 2015 [13]. LRTI are common and foremost causes of death in children worldwide [14, 15, 16, 17, 18, 19]. Another study showed that, LRTIs are one of the leading causes of morbidity and mortality among children [20, 21] in both developed and developing countries. LRTIs are common diseases in children under five globally [22, 23, 24, 25], accounting for high morbidity, hospital admissions, and healthcare expenditures, especially in emerging countries [26, 27, 28]. LRTI in children are often below the level of the larynx and may be taken as Broncho-pneumonia, pneumonia, bronchiolitis and bronchitis [29, 30, 31]. Every year, 3% of all children less than 12 months of age need to be admitted for moderate or severe LRTI [32, 33, 34, 35].
Recent studies from the World Health Organization (WHO) suggest that Acute Lower Respiratory Tract Infections (ALRTI) is accountable for 20% of deaths in under five years old children, every year. About 120–156 million cases of ALRI occur globally, and almost 1.4 million deaths occur every year. More than 95% of these deaths occur in underdeveloped and developing countries [36, 37].
The current study was conducted on different types of LRTI in children less than five years of age in Lahore, based on disease year, age, gender, locality, and seasonal distribution of disease. This paper will help to design other research studies on the prevalence of LRTIs in children aged <2-5 years.
Material and methods.
Selection of study area
This study was conducted in Lahore, according to census of 2017, the population of Lahore was 11,126,285 (PBOS, 2017). Lying between 31°15′—31°45′ N and 74°01′—74°39′ E, Lahore is surrounded on the north and west by the Sheikhupura district, on the east by Wagah, and on the south by Kasur District. Ravi River flows on the northern side of Lahore. The weather of Lahore is extreme during the months of May, June, and July, when the temperatures soar to 40–48 °C (104–118 °F). The lowest temperature recorded in Lahore is −1.1 °C (30 °F) (WCLA, 2012).
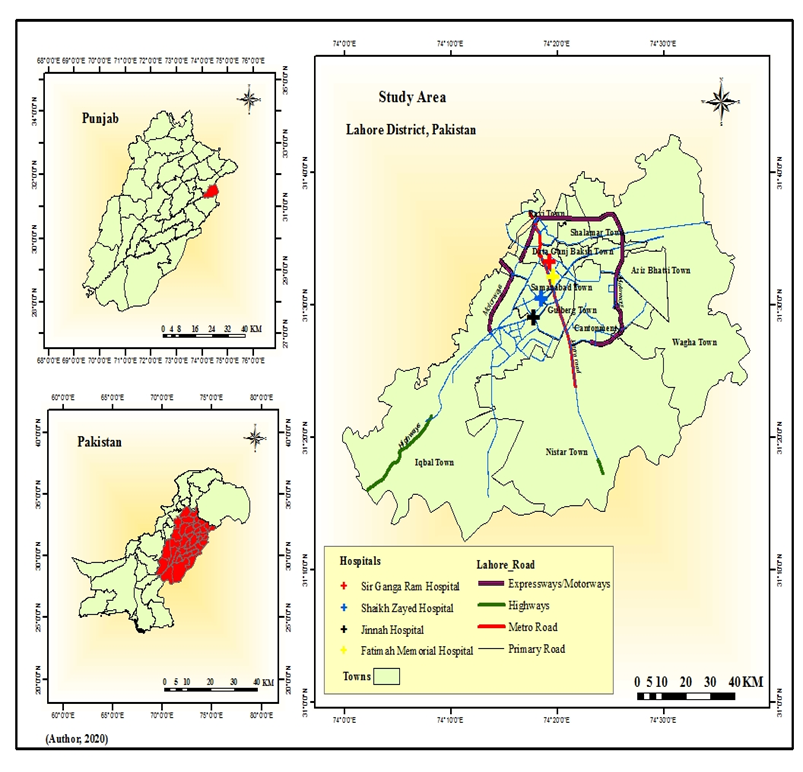
Figure 1. The Study area.
Data collection and analysis
Following the nature of the study, secondary data sources were collected. This study was conducted for children under 5 years of age admitted with LRTI illness at Fatima memorial hospital, Jinnah hospital, Sir Ganga Ram hospital, and Sheikh Zaid hospital of Lahore from the year 2017-2021. After taking permission from the institutional ethical committee, all children with LRTI were included in the study. A standardized Performa was designed and then the medical records of the hospitals were reviewed to collect individual’s data regarding age, gender, and area of residence, diagnosis of disease, seasonal distribution of disease, and date of hospital admission. The collected information was organized and tabulated in Microsoft Excel 13. Data was analyzed using IBM SPSS 22. To analyze the results, the chi-square test (P<0.05) was applied to assess the association between these variables (disease and age, disease and gender, disease and season). A P-value of 5% (2-tailed) level of significance was considered statistically significant. Afterward for the mapping technique, ArcGIS 10.5 were used.
Results and discussion.
LRTI are mainly responsible for the continuing high rates of morbidity and mortality in children under 5 years in developing countries, accounting for more than 4 million deaths per year. The findings in table 1 and figure 2 revealed that the higher morbidity of LRTI was in 2021. The mean of data was computed as 2019.05 and the standard deviation was 0.81. The trend of LRTI was observed increasing (2017-2021) gradually.
Table 1. Year of admission
| Year Frequency | Percent | |||
| 2017 | 796 | 30.5% | ||
| 2019 | 891 | 34.2% | ||
| 2021 | 922 | 35.3% | ||
| Total | 2,609 | 100.0 | ||
Source: Field survey, 2020
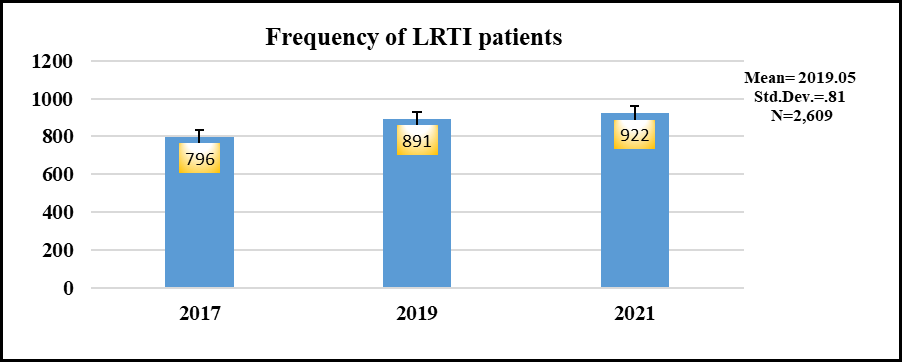
Figure 2. The frequency of LRTI disease in Lahore district for the last three years 2017-2019.
Table 2. Town wise & disease wise patterns of LRTI in children
| Sr. no | Towns | Broncho-pneumonia | Pneumonia | Bronchitis | Bronchiolitis | Total | |
| 1 | Allama Iqbal Town | 720 | 55 | 47 | 155 | 977 | 37% |
| 2 | Samna bad Town | 319 | 37 | 4 | 42 | 402 | 15% |
| 3 | Gulberg Town | 172 | 20 | 14 | 25 | 231 | 9% |
| 4 | Data Gung Bakhsh | 318 | 19 | 16 | 34 | 387 | 15% |
| 5 | Aziz Bhatti Town | 85 | 3 | 4 | 8 | 100 | 4% |
| 6 | Ravi Town | 120 | 9 | 1 | 12 | 142 | 6% |
| 7 | Nishter Town | 84 | 6 | 4 | 16 | 110 | 4% |
| 8 | Cantonment | 65 | 12 | 6 | 6 | 89 | 3% |
| 9 | Shalimar Town | 101 | 13 | 2 | 5 | 121 | 5% |
| 10 | Wahga Town | 38 | 5 | 1 | 6 | 50 | 2% |
| Total | 2022 | 179 | 36 | 309 | 2609 | 100 |
Source: Field survey, 2020
Town wise distribution of LRTI patients.
Figure 3 illustrates the spatial distribution of LRTI cases in the study site. The reported 2,609 patients of LRTI were observed during the study period in all towns of Lahore. Out of 2,609 cases, 977 (37%) were found in Allama Iqbal Town with the maximum number of LRTI, Samnabad town with 402 cases (15%), Data Gunj Bakhsh Town with 387 (15%) cases. The minimum number of cases were seen in Wahga Town with 50 patients (2%). The further geographical situation of the diseases can be seen through pie charts in Figure 3 & 4.
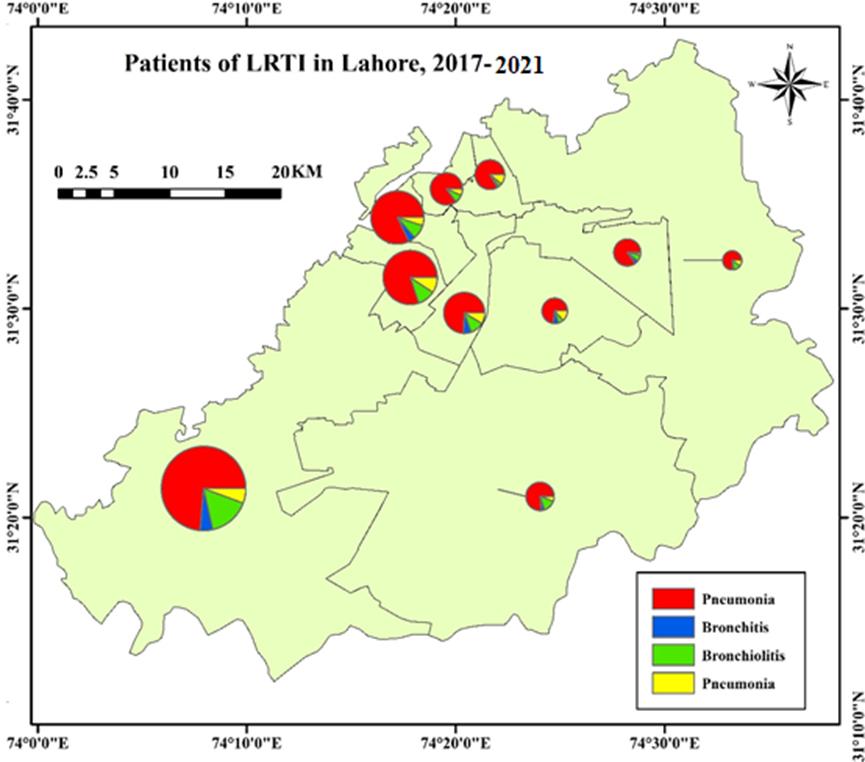
Figure 3. Town wise & disease wise patterns of LRTI.

Figure 4. Town wise spatial distribution of disease.
Table 3. Children hospitalized with LRTIs in 2017-2021, per season of the year
| Condition | Winter | % | Spring | % | Summer | % | Autumn | % | Total | % | |
| Broncho-pneumonia | 1032(64.9) | 79 | 362(25.0) | 72 | 183(10.1) | 74 | 445(22) | 81.6 | 2022(100) | 77.4 | |
| Pneumonia | 74(42) | 5 | 56(31) | 11 | 20(11) | 8 | 29(16) | 5.5 | 179(100) | 6.9 | |
| Bronchitis | 29(30) | 2 | 28(28) | 5.5 | 23(23) | 9.5 | 19(19) | 3.4 | 99(100) | 3.8 | |
| Bronchiolitis | 177(57) | 14 | 59(19) | 11.5 | 21(7) | 8.5 | 52(17) | 9.5 | 309(100) | 11.8 | |
| Total | 1312 | 100 | 505 | 100 | 247 | 100 | 545 | 100 | 2609 | 100 |
Source: Field survey, 2020
While observing the seasonal variations, about 1312 cases were observed in Dec-Feb, 545 cases from Sep-Nov and 505 cases for Mar-May. The lease number of cases were recorded in June-Aug which were 247.
Figure 5 demonstrates the seasonal comparison of Bronchopneumonia, Bronchitis, and Bronchiolitis, and Pneumonia. Concerning the seasons, the largest number of cases of LRTI, were observed in winter season. Bronchopneumonia on first, followed by Bronchiolitis, Pneumonia was the third in the number of cases, and Bronchitis was with fewer cases.
Chi-square analysis was performed to check the association between disease and season (Table 4&5).
Table 4. Association between disease and seasons of the year
| Value | df | Asymp. Sig. (2-sided) | |
| Pearson Chi-Square | 2636.469 | 9 | .000 |
| Likelihood Ratio | 2724.244 | 9 | .000 |
| Linear-by-Linear Association | 1792.671 | 1 | .000 |
| No of Valid Cases | 2609 |
Table 5. Symmetric Measures
| Value | Approx. Sig. | |||
| PhiCramer's V | 1.005 | .000 | ||
| .580 | .000 | |||
| 2609 | ||||
The output of Table 4 shows that significant association found in disease and season of the year with P-value (0.00)). The value of Phi (1.005) in table 5 also showed a strong association between the variables.
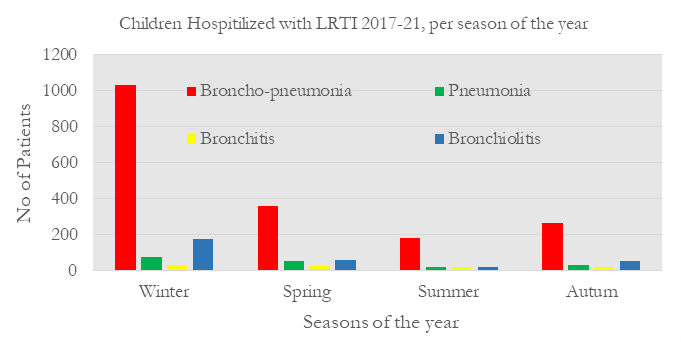
Figure 5. Children hospitalized with LRTI 2017-2021, per season of the year.
Table 6. Children hospitalized with LRTIs in 2017, 2019, 2021, per age groups
| Condition | <2m | 2-12m | 13-24m | 25-60m | Total | |||||
| No | % | No | % | No | % | No | % | No | % | |
| Bronchopneumonia | 209 | 73(10.3) | 1425 | 77(70.4) | 229 | 79(11.3) | 159 | 80(7.8) | 2022100 | 77 |
| Pneumonia | 18 | 6(10) | 123 | 8(69) | 23 | 8(13) | 15 | 8(8) | 179100 | 7 |
| Bronchitis | 11 | 4(11) | 73 | 4(74) | 7 | 2(7) | 8 | 4(8) | 99100 | 4 |
| Bronchiolitis | 48 | 17(16) | 213 | 11(69) | 32 | 11(10) | 16 | 8(5) | 309100 | 12 |
| Total | 286 | 100 | 1834 | 100 | 291 | 100 | 198 | 100 | 2,609 | 100 |
Source: Field survey, 2020
Considering age, there was a significant difference between the age groups. Table 6 and figure 6 shows the age group dissemination of LRTI among children. A high incidence of LRTI patients was seen in 2-12m age with number (1834) patients. Broncho-pneumonia was the most common entity related to LRTI (70.4%) and most commonly seen in the age group of 2-12m (1425cases). The second group comprised of 13-24m of age with 291 cases. Out of 291 cases, 229 cases of Broncho-pneumonia were found in this age group. The third group is <2m, with 286 patients. The last group was 25-60m, where minimum number of pediatrics found in this group were found with 198 cases.
Chi-square analysis was performed to check the association between disease and age groups (Table 7&8).
Table 7. Association between disease and age groups
| Value | df | Asymp. Sig.(2-sided) | |
| Pearson Chi-Square | 4832.599a | 9 | .000 |
| Likelihood Ratio | 3052.812 | 9 | .000 |
| Linear-by-Linear Association | 2014.410 | 1 | .000 |
| No of Valid Cases | 2609 |
Table 8. Symmetric Measures
| Value | Approx. Sig. | ||
| Phi | 1.361 | .000 | |
| Cramer's V | .786 | .000 | |
| 2609 | |||
The output of Table 6 shows that a significant association was found between disease and age groups with P-value (0.00). The value of Phi (1.361) in table 7&8 showed a strong association between the variables.

Figure 6. Children hospitalized with LRTI, per age group
Table 9. Cross-Tabulation analysis of Children hospitalized with LRTI, according to gender
| Disease | Gender | Total | |
| Male | Female | ||
| Broncho-pneumonia | 1289 | 733 | 2022 |
| 63.7% | 36.3% | 100.0% | |
| Bronchitis | 49 | 50 | 99 |
| 49.5% | 50.5% | 100.0% | |
| Bronchiolitis | 188 | 121 | 309 |
| 60.8% | 39.2% | 100.0% | |
| Pneumonia | 126 | 53 | 179 |
| 70.4% | 29.6% | 100.0% | |
| Total | 1652 | 957 | 2609 |
| 63.3% | 36.7% | 100.0% | |
Source: Field survey, 2020
Table 9 shows the gender variation of disease in children. This study was done among 2,609 children in the age group under five years of LRTI. A higher proportion of males 63.3% were reported to have LRTI when compared to females with 36.7%.
The study carried out by Savitha AK, Gopala Krishnan S, 2019, reported that male children are more prone to LRTI when compared to female children. The probable reason that there is predominance among male children could be because of the tendency of male children to play outside the home gets them exposed to infected aerosols from the surrounding outdoor environment when compared to female children. There is a huge male predominance observed as shown in figure 7 and table 9.
Chi-square analysis was performed to check the association between disease and gender (Table 10&11).
Table 10. Association between disease and gender
| Value | Df | Asymp. Sig. (2-sided) | |
| Pearson Chi-Square | 12.978a | 3 | .005 |
| Likelihood Ratio | 12.792 | 3 | .005 |
| Linear-by-Linear Association | .148 | 1 | .700 |
| No of Valid Cases | 2609 |
Table 11. Symmetric Measures
| Value | Approx. Sig. | ||
| PhiCramer's V | .071 | .005 | |
| .071 | .005 | ||
| 2609 | |||
The output of Table 11 shows that a significant association was found between disease and gender with P-value (0.05)). The value of Phi (.071) in table 9&10 also showed a strong association between the variables.

Figure 7. Children hospitalized with LRTI 2017-2021, according to gender.
It was necessary to examine the possible relationship between respiratory disease and age, gender and season. For this purpose, few statistical tests i.e., multiple linear regression and ANOVA were performed. A strong correlation was found among the variables (Table 12).
Table 12. Summary of statistics model of fitness
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate | Durbin-Watson | |
| 1 | .916 | .840 | .840 | .380 | .024 |
Table 13. Analysis of variance (ANOVA)
| Model | Sum of Squares | df | Mean Square | F | Sig |
| Regression | 1967.758 | 3 | 655.919 | 4550.208 | .000 |
| Residual | 375.515 | 2605 | .144 | ||
| Total | 2343.273 | 2608 |
Multiple Linear regression analysis and ANOVA were conducted to examine the relationship between respiratory diseases as a dependent variable and age, gender, and season as independent variables. Table 12 summarized the descriptive statistics and analysis results. The results indicated that the age, gender and season was significant predictor of respiratory diseases, F (3, 2608) =4550.208, Sig=.000. Moreover, the Durbin Watson value i.e., .024 indicate a positive autocorrelation as it is less than 2.
Conclusion.
Childhood respiratory infections are a major concern in developing countries. The present study concludes that the Lahore district has witnessed substantial growth in the incidence and prevalence of LRTI, types during 2017, 2019, and 2021. In year-wise analysis, maximum number of patients were seen in 2021. In the town-wise distribution of patients, the greater number of LRTI cases were seen in Allama Iqbal Town with 2022 cases. In the next analysis, there was a huge male predominance observed in our study. The study was done by Srinivasa & Patel (2018) which includes children less than 5 years also showed male predominance. The most common age group in the study was 2-12m followed by the13-24m group. Among LRTI in children, most of the cases were bronchopneumonia followed by bronchiolitis, pneumonia and bronchitis. Mungala VK et al also reported bronchopneumonia as the commonest LRTI in their study. In another study by Begum, J et al., (2018) in developing countries Bronchiolitis and Bronchopneumonia are the major contributing respiratory illness. The seasonal variation of the disease varies from season to season and area to area. In this study a larger number of cases were observed in the winter season (Dec-Feb) followed by autumn (Sep-Nov), spring (Mar-May), and summer (Jun-Aug). Chi-square, multiple linear regression analysis, and ANOVA was applied to check the association of respiratory diseases between the variables. There is a strong association between disease and season, disease and gender and disease and age groups. An epidemiological outline of admissions for respirational infections in this population, highlighting the periods of the year and the most vulnerable age groups, will lead to protective measures that can be applied to prevent hospitalizations for these various illnesses.
Acknowledgement.
The authors thank to Dr Iqbal Bano head of the Institute of Children Hospital Lahore (ICHL) for data availability.
Author’s contribution.
The authors made considerable contributions to beginning, analysis and interpretation of data; took part in drafting the article or reviewing it critically for important logical content; gave final consent of the version to be published; and agree to be accountable for all aspects of the work.
Conflicts of interest. The authors declare no conflicts of interest regarding the publication of this paper.
REFERENCES
- Abdel Mohsen, A., Amin, M., Yousef, R. “Acute Respiratory Tract Infection in Children under Five- Year; Study of Prevalence, Risk Factors and Outcome in Minia University Children’s Hospital, Egypt”. “International Journal of Pediatrics”, 2020, 8(4), 11149-11157. doi: 10.22038/ijp.2019.42502.3567.
- Adane, M. M., Alene, G. D., Mereta, S. T., & Wanyonyi, K. L. “Prevalence and risk factors of acute lower respiratory infection among children living in biomass fuel using households: a community-based cross-sectional study in Northwest Ethiopia”. “BMC Public Health”, 2020 20(1), 363. Doi: 10.1186/s12889-020-08515-w.
- Alemayehu, S., Kidanu, K., Kahsay, T. et al. “Risk factors of acute respiratory infections among under five children attending public hospitals in southern Tigray, Ethiopia, 2016/2017”. “BMC Pediatr”, 2019, 19,380 (2019). https://doi.org/10.1186/s12887-019-1767-1.
- Akand, N., Sarkar, P. K., Alam, M. J., Selim, A. S. M., Rahman, M., & Debnath, S. “Anemia: A Risk Factor for Acute Lower Respiratory Tract Infection in Children under 5 years of age” 2019.
- Begum, J., Mamun, M. A., Sultana, A., Kamruzzaman, M., Imran, A., & Nahar, M. L. “Pattern of Respiratory Diseases among Admitted Children in Pediatric Pulmonology Unit: A Tertiary Center Experiences”. “Northern International Medical College Journal”,2018, 9(2), 308-310. https://doi.org/10.3329/nimcj.v9i2.38913.
- Brijesh Sathian, Asis De, Padam Simkhada, Kalpana Malla, Arnab Ghosh, Indrajit Banerjee, Bedanta Roy, H S Supram, Elayedath Rajesh, and Suresh Devkota. “Time Trend of Pneumonia in under Five Children of Nepal.” “American Journal of Public Health Research”, 2015, vol. 3, no. 4A (2015): 27-30. doi: 10.12691/ajphr-3-4A-5.
- Chungkham Bidyarani Devi et al. “A study to Assess the Prevalence of Upper Respiratory Tract Infection (Urti) and its Risk Factors Among Children in Selected Hospital, Guwahati, Assam”. “Int J Recent Sci Res”. 2018, 9(6), pp. 27643-27646. DOI: http://dx.doi.org/10.24327/ijrsr.2018.0906.2302.
- Cohen, C., Moyes, J., Tempia, S., Groome, M., Walaza, S., Pretorius, M. . . . Madhi, S. A. “Epidemiology of Acute Lower Respiratory Tract Infection in HIV-Exposed Uninfected Infants”. “Pediatrics”,2016, 137(4), e20153272. doi:10.1542/peds.2015-3272.
- David M le Roux, Mark P Nicol, Landon Myer, Aneesa Vanker, Jacob A M Stadler, Eckart von Delft, Heather J Zar. “Lower Respiratory Tract Infections in Children in a Well-vaccinated South African Birth Cohort: Spectrum of Disease and Risk Factors”, “Clinical Infectious Diseases”, 1 November 2019, Volume 69, Issue 9, Pages 1588–1596, https://doi.org/10.1093/cid/ciz017.
- Gaston Ofman, Brad Pradarelli, Mauricio T Caballero, Alejandra Bianchi, Luciano Alva Grimaldi, Andrea Sancilio, Karina Duenas, Andrea Rodriguez, Fernando Ferrero, Adrian Ferretti, Silvina Coviello, Fausto M Ferolla, Patricio L Acosta, Eduardo Bergel, Romina Libster, Fernando P Polack. “Respiratory Failure and Death in Vulnerable Premature Children with Lower Respiratory Tract Illness”, “The Journal of Infectious Diseases”, 2020, jiaa046, https://doi.org/10.1093/infdis/jiaa046.
- González-Ortiz, A. M., Bernal-Silva, S., Comas-García, A., Vega-Morúa, M., Garrocho-Rangel, M. E., & Noyola, D. E. “Severe Respiratory Syncytial Virus Infection in Hospitalized Children”. “Archives of Medical Research”, 2019, 50(6), 377-383. doi: https://doi.org/10.1016/j.arcmed.2019.10.005.
- Green, R. J., Zar, H. J., White, D. A., & Madhi, S. A. “Viral Lower Respiratory Tract Infections”. “Viral Infections in Children”, 2017, Volume II, 27–56. https://doi.org/10.1007/978-3-319-54093-1_2.
- Kini, S., Kalal, B. S., Chandy, S., Shamsundar, R., & Shet, A. “Prevalence of respiratory syncytial virus infection among children hospitalized with acute lower respiratory tract infections in Southern India”. “World journal of clinical pediatrics”, 2019, 8(2), 33–42. https://doi.org/10.5409/wjcp.v8.i2.33
- Kishamawe, C., Rumisha, S.F., Mremi, I.R., Bwana, V.M., Chiduo, M.G., Massawe, I.S. and Mboera, L.E.G. “Trends, patterns and causes of respiratory disease mortality among inpatients in Tanzania, 2006–2015”. “Trop Med Int Health”, 2019, 24: 91-100. Doi: 1111/tmi.13165.
- Krishnan, A., Kumar, R., Broor, S., Gopal, G., Saha, S., Amarchand, R., Choudekar, A., Purkayastha, D. R., Whitaker, B., Pandey, B., Narayan, V. V., Kabra, S. K., Sreenivas, V., Widdowson, M. A., Lindstrom, S., Lafond, K. E., & Jain, S. “Epidemiology of viral acute lower respiratory infections in a community-based cohort of rural north Indian children”. “Journal of global health”,2019, 9(1), 010433. https://doi.org/10.7189/jogh.09.010433
- Kumar, S. G., Majumdar, A., Kumar, V., Naik, B. N., Selvaraj, K., & Balajee, K. “Prevalence of acute respiratory infection among under-five children in urban and rural areas of Puducherry, India”. “Journal of natural science, biology, and medicine”, 2015, 6(1), 3–6. https://doi.org/10.4103/0976-9668.149069
- Mathew, E. A., Koshy, N., Telaprolu, M., Mahendravarman, P., & Vinoth, S. “Assessment of patient compliance with antibiotic treatment for lower respiratory tract infection in children”. “Age”,2019, 9(12years), 6.
- Mohsen, A. A., Amin, M., & Yousef, R. “Acute Respiratory Tract Infection in Children under Five-Year”; “Study of Prevalence, Risk Factors and Outcome in Minia University Children’s Hospital, Egypt” 2020.
- Muhanuzi, B., Sawe, H.R., Kilindimo, S.S. et al. “Respiratory compromise in children presenting to an urban emergency department of a tertiary hospital in Tanzania: a descriptive cohort study”. “BMC Emerg Med”2019, 19, 21 https://doi.org/10.1186/s12873-019-0235-4
- Munagala VK, Mahesh RMU, Kandat J, Ponugoti M. “Clinical study of lower respiratory tract infections in children attending a tertiary care hospital”. “Int J Contemp Pediatr”2017; 4:1733-8.
- Naz, R, Gul, A, Javed, U, Urooj, A, Amin, S, Fatima, Z. “Etiology of acute viral respiratory infections common in Pakistan”: “A review. Rev Med Virol”.2019; 29: e2024. https://doi.org/10.1002/rmv.2024
- Orimadegun, A. E., Adepoju, A. A., & Myer, L. “A Systematic Review and Meta-analysis of Sex Differences in Morbidity and Mortality of Acute Lower Respiratory Tract Infections among African Children”. “JPR”2020, 8(2), 65-78. doi:10.32598/jpr.8.2.65
- Papanikolaou, I. C., & Tsenempi, X. A. “Tropical Lung Diseases. Hunter's Tropical Medicine and Emerging Infectious Diseases”, 2020 (Tenth Edition) (pp. 1-7).
- Photis YN. “Disease and Health Care Geographies”: “Mapping Trends and Patterns in a GIS, Jordan”. Health Sci J. 2016, 10:3.
- Rehman, Gulalai & Kakar, Allauddin & Zarak, Muhammad Samsoor. “PREVALENCE OF RESPIRATORY TRACT INFECTIONS IN CHILDREN UNDER FIVE YEARS AT QUETTA”. “International Journal of Current Research” 10.24941/ijcr.32359.09.2018.
- Reiner, R.C., Welgan, C.A., Casey, D.C. et al. “Identifying residual hotspots and mapping lower respiratory infection morbidity and mortality in African children from 2000 to 2017”. “Nat Microbiol4, 2310–2318”2019. https://doi.org/10.1038/s41564-019-0562-y.
- Srinivasa, S., PATEL, Shruthi. “A study on distribution pattern of lower respiratory tract infections in children under 5 years in a tertiary care Centre. International”. “Journal of Contemporary Pediatrics”
- Savitha AK., Gopalakrishnan S. “Determinants of acute respiratory infections among under five children in a rural area of Tamil Nadu, India”. “J Family Med Prim Care”2018; 7:1268-73. DOI: 10.4103/jfmpc.jfmpc_131_18
- Shoukat, N., Kakar, A., Shah, S. A., & Sadiq, A.,2019. “Upper respiratory tract infections in children age 2 to 10 years in Quetta”: A prevalence study”. “Pure and Applied Biology (PAB)”, 8(2), 1084-1091.
- Seidu, A.A., Dickson, K. S., Ahinkorah, B. O., Amu, H., Darteh, E. K. M., & Kumi-Kyereme, A. “Prevalence and determinants of Acute Lower Respiratory Infections among children under-five years in sub–Saharan Africa: Evidence from demographic and health surveys”. “SSM - Population Health”, 2019, 8, 100443. doi: https://doi.org/10.1016/j.ssmph.2019.100443
- Sricharoenchai S., Palla, E., Sanicas, M. “Seasonality of Respiratory Syncytial Virus - Lower Respiratory Tract Infection (RSV-LRTI) in Children in Developing Countries” 2016. DOI: 15406/jhvrv.2016.03.00076
- Tazinya, A. A. “Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon”. “BMC Pulmonary Medicine”, 2018 doi:DOI 10.1186/s12890-018-0579-7.
- Thukral, S., & Saxena, S.,2019. “PREVALENCE OF LOWER RESPIRATORY TRACT INFECTION AMONG PATIENTS IN A TERTIARY CARE HOSPITAL IN NORTH INDIA”. “Plant Archives”,19(2), 2191-2194.
- Troeger, C. E., Khalil, I. A., Blacker, B. F., Biehl, M. H., Albertson, S. B., Zimsen, S. R. M., Reiner, R. C. “Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: an analysis for the Global Burden of Disease Study 2017”. “The Lancet Infectious Diseases”, 2020, 20(1), 60-79. doi: https://doi.org/10.1016/S1473-3099(19)30410-4
- United Nations Children’s Fund The state of the world's children: A fair chance for every child. UNICEF,New York (2016).
- Wang, X., Li, Y., O'Brien, K. L., Madhi, S. A., Widdowson, M.-A., Byass, P., Nair, H. “Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study”. “The Lancet Global Health”, 2020 8(4), e497-e510. doi: https://doi.org/10.1016/S2214-109X(19)30545-5
- Wheeler, Dennis, Gareth Shaw, and Stewart Barr. “Statistical techniques in geographical analysis”. “Routledge”,