The Safeguard measures for mitigating the impact of COVID-19 on radiotherapy services in a Cancer Hospital: A resource-constrained approach
Attia Gul1, Muhammad Mubashar Hussain1, Musab Riaz1, Nazia Neelam Shehzadi1
1 Atomic Energy Cancer Hospital, Institute of Nuclear Medicine, Oncology & Radiotherapy (INOR), Abbottabad 22010, Pakistan.
* Correspondence: Attia GUL, attiagul@gmail.com
Citation |Gul. A, Hussain. M. M, Riaz. M, Shehzadi. N. N, “The Safeguard measures for mitigating the impact of COVID-19 on radiotherapy services in a Cancer Hospital: A resource-constrained approach”. International Journal of Innovations in Science and Technology. Vol 4, Issue 1, 2022, pp: 266-275.
Received | Jan 21, 2022; Revised | Feb 13, 2022 Accepted | March 08, 2022; Published | March 09, 2022.
T
his article suggests the preventive measures for healthcare department (particularly his article suggests the preventive measures for healthcare department (particularly radiotherapy department) to reduce the probability of corona virus transmission with a resource constrained approach without affecting the work flow. COVID-19 has affected the patients as well as staff of radiotherapy department leaving a severe negative impact on the financial resources of INOR cancer hospital, Abbottabad. Multiple preventive measures have been taken to reduce the probability of spreading the coronavirus while pursuing the timely treatment of radiotherapy patients without compromising their oncological outcomes. In this context, a triage center was established to filter out the Covid suspected/confirmed patients to reduce the risk of infection to other patients and staff. Social distancing was ensured by making amendments in patient gathering areas. Also extensive ventilation and disinfection procedures were adopted to clean the surfaces. Following these measures, patient flux did not show any considerable decrease in second, third and fourth wave as compared to first wave when patient flux reduced to about less than 25 %. Preventive measures were also taken for the employees by ensuring them to wear personal protective equipment during office hours. To further reduce the probability of contact, telemedicine was adopted for patients where possible. All employees were made to be fully vaccinated by July 2021 resulting in 100 % reduction in new cases among INOR employees in the following fourth COVID wave. Owing to these stringent measures taken to fight against coronavirus, ratio of contracting the coronavirus among the employees and patients of INOR has been found <10% overall in this pandemic, While no mortality has been reported so far.
Keywords: COVID-19, Radiotherapy, Precautionary measures, Resource-constrained approach, Healthcare department.
|
Author’s Contribution. Attia GUL: Writing of manuscript, Theory, Data Analysis Muhammad Mubashar HUSSAIN: Theory, Data Collection and Data Analysis. Musab RIAZ: Basic Idea, Manuscript Review Nazia Neelam SHEHZADI: Theory, Data Collection |
Conflict of interest. There is no conflict of interest to disclose.
|
Project details. NA
|
Introduction
The outbreak of coronavirus infectious disease 2019 (COVID-19) has badly affected the daily life of people worldwide and transformed the working practice of almost all the departments. As of February 05, 2022, more than 380 million confirmed cases of Covid-19 (death toll > 5.7 million) have been reported globally [1], of which more than 1.4 million (death toll >29,000) have been reported in Pakistan [2]. Another major concern is the rapid transmission of this infectious disease and is about three times more infectious than flu. While approximately 25 % of transmitted cases remain asymptomatic and cause silent transmission to about 10 % cases [3]. Till now, four waves of coronavirus have been out broken, while concern of facing the fifth wave have grown amid the surging infections across the world due to emergence of the omicron variant, a strain of the virus first identified in South Africa. Omicron has been reported to be more transmissible as compared to other variants and 2.7-3.7 times as infectious as delta variant among the vaccinated population [4]. Though, it is less severe but should not be considered as “mild” and also causes reinfection in people who had contracted other variants previously.
The oncology and radiotherapy departments have been greatly impacted as the cancer patients are more vulnerable to highly infectious COVID-19 owing to their immunocompromised state and frequent visits of hospitals and other medical facilities. An optimized approach is required for the management of cancer patients to protect them from this fatal disease as well as their timely treatment without compromising oncological outcomes. This situation has caused a transformation of working practice in the cancer care discipline worldwide. “This pandemic has meant a transformation of every aspect of cancer care, irrespective of treatment, inpatient or outpatient, and radical or palliative intent”, as quoted by James Spicer (Guy’s and St Thomas’ Hospital NHS Foundation Trust in London) [5].
A Significantly high rate of mortality has been reported among COVID-19 patients who were having cancer [6]. Liang et al have reported that the cancer patients are relatively at higher risk of having severe events (ICU admission, Intubation, or death: 39 % vs. 8 %, p<0.001) [7]. This requires the stringent measures to be taken for stopping the spread of coronavirus in these immunocompromised patients. The effect of anticancer treatments, Lee at al have conducted a study and reported that the mortality from COVID-19 in cancer patients is driven mainly by age, gender and other comorbidities like hypertension and cardiovascular disease. However, no significant effect of chemotherapy, immunotherapy, hormonal therapy, targeted therapy, radiotherapy or other anticancer treatment has been observed on the mortality rate of COVID-19 patients [8]. This study suggests that anticancer treatments should not be unnecessarily postponed in COVID-19 patients. Considering the deleterious effects of delaying radiotherapy, Nagar et al suggested that radiotherapy can safely be delivered during COVID-19 pandemic mostly with hypofractionated regimes (with larger but fewer fractions) while following the precautionary measures for safe contact with patients [9].
The ongoing public health emergency has also affected the Oncology departments in Pakistan. This article addresses the impact of COVID-19 on the Institute of Nuclear medicine, Oncology and Radiotherapy (INOR) from different aspects particularly emphasizing its radiotherapy services and the safeguard measures taken to mitigate its effect on cancer patients and working staff during this whole pandemic. To the best of our knowledge, the effect of employing the low cost commonly recommended preventive measures in a radiotherapy department has not been reported so far. In general, this article provides a latest comprehensive guideline with resource constrained approach to minimize the chance of contracting the coronavirus in current and upcoming corona waves.
Overview of INOR
INOR is the public cancer hospital situated in Abbottabad, a city of the province Khyber Pakhtoon khaw (KPK) in Pakistan. It provides nuclear medicine, radiological and oncological services to the cancer patients with limited budget. A total of 126 Employees (including medical and paramedic staff) are working at INOR to serve more than 20,000 patients annually. Indoor facility is also available for patients from the far-flung areas.
Methodology
Safeguard Measures for Radiotherapy
Considering the safety of staff and the other patients, in the early first wave, (from late March to the end of May 2020), radiotherapy services to new patients was halted at INOR, while the ongoing radiotherapy courses left uninterrupted to avoid the treatment gap and the related complexities. However, patients with palliative radiotherapy (mostly with one fraction) were entertained.
Radiotherapy for breast cancer shares the major flux of patients (around 30 %) in the department. The radiotherapy for these patients also requires the considerable time due to the complexity in the setup as well as larger number of fields with more than one isocenter (Two tangential fields and one or two supra clavicular fields) as compared to other cancers. Therefore, these patients require special consideration for reducing the probability of spreading the infection. Considering the larger fraction long time of treatment required for these patients, a hypofractionated protocol of 40.5 Gy in 15 fractions was already being followed at INOR (instead of standard protocol of 50 Gy in 25 fractions). The same hypofractionated protocol has been recommended in the “International Guidelines on Radiation Therapy for Breast Cancer During the COVID-19 Pandemic” [10].
Ventilation
As a general precaution to minimize the corona virus transmission, natural ventilation like window opening is suggested when appropriate to do so. As per manufactory recommendations, it is recommended to run the heating, ventilation and air conditioning system (HVAC) system at maximum outside airflow for 2 h before and after spaces are occupied. Routine maintenance of HVAC systems must be ensured to meet the industry standards. To ensure good indoor ventilation, WHO ventilation roadmap is an important resource in context of COVID-19 [11].
During all Covid waves, extensive ventilation was ensured at INOR. For this purpose, specially designed large exhaust fans were installed in patients waiting areas and general wards. To ensure excessive ventilation, some patient waiting areas were also shifted to open areas outside the main covered building of the hospital, where the installation of exhaust fans was not feasible. The windows of offices and corridors were used to remain opened during working hours of hospital.
Physical distancing
Measures were introduced to maintain safe physical distancing according to the national regulations between people by discouraging social gatherings and direct physical contact with other persons, regulating entrance to non-workers, implementing stringent control over external access, scheduling queuing times, enforcing queue management via marking on the floor, decreasing workspace density and implementing physical barriers. By encouraging teleconferences, need of physical meetings were minimized. Exit times and workplace entrance were staggered to evade gathering. The staff strength was reduced to 50 % during Covid to manage physical distancing in the office vans of INOR for employees coming from far flung areas. To evade the public transport further, substitutive ways of transportations like using a personal vehicle, biking or walking were encouraged [12].
Furthermore, to ensure the physical distancing, seating arrangement for patients was modified accordingly during Covid. The oncologists’ desks were separated by fixing transparent sheets as physical barriers around the desk in the OPDs for patients’ consultation. At reception desk, floor was marked to ensure that the patients are queued with at least 6 ft. distance. Number of entrance and exit gates in the main building was also increased to avoid gathering on the gates. Furthermore, all the physical meetings and seminars were postponed or replaced with online meetings.
Hand hygiene
Alcohol-based hand sanitizer or conveniently located hand washing stations are recommended to be implemented at all bathrooms, entrances, dining facilities and workstations to encourage frequent hand washing/sanitizing [13]. To comply with this preventive measure, hand sanitizers were made available in all offices, corridors, reception desks, wards, bath rooms etc. The signs/posters were placed at different locations to remind the employees for appropriate hand hygiene. It was mandatory for all the workers and patients to sanitize their hands at the entrance of the workspace.
Cleaning and disinfection of equipment/environmental surfaces
To minimize the corona virus transmission, high touch surfaces and high traffic areas like main corridors are suggested be cleaned and disinfected on priority basis, several times daily. In this regard, standard operating procedures were followed at INOR as per the recommendation of WHO [14, 15]. The detergent and water was used to clean the surfaces (specially the floor) for removing the organic matters on daily basis. Common bleach (sodium hypochlorite) solution with concentration of 0.5 % (5000 ppm) was used for cleaning the surfaces and floor mopping at least twice a day. Whereas 80 % ethyl alcohol solution, as suggested by Cirrincione et al [16], was used for cleaning the equipment with special consideration of high touch surfaces like, hand pendants, treatment head, consoles, and couches of radiotherapy machines. It was ensured that the application and preparation of disinfection solutions was according to the instructions of manufacturer to care for the health and safety of disinfection workers. For this purpose, 2-3 workers from each department were trained for safe handling of disinfectants [16].
Personal protective equipment (PPE)
During Covid pandemic, All the employees were provided with optimal Personal Protective Equipment (PPEs) free of cost based on their exposure to the patients and general public., PPEs included masks, gowns, head covers, gloves and shoe covers. It was mandatory to use double masks (inner non-medical cloth mask with outer N95 respirator) for the employees directly dealing and handling the patients. Whereas wearing inner fabric mask with outer medical (surgical) mask was compulsory for all other workers working in close proximity to co-workers and clients. Special lectures were arranged for INOR employees on WHO recommendation of how and when to use masks [17].

Figure 1. Radiotherapy Technologists wearing PPEs and working on CT simulator (Left), CT simulator console (Middle) and Cobalt-60 teletherapy machine (Right).
General Measures for Working Staff
As preliminary measures to minimize the spread of Covid-19, staff of INOR was reduced under the policy of cautionary isolation. Initially, the workforce was reduced to 50 % (in late March and early April 2020) and then further shrank to the bare minimum skeleton staff till the end of May 2020. Workers with age >50 years as well as pregnant ladies were exempted from duty in the first wave of coronavirus. From June 2020 onwards, INOR had started to work with full capacity and all the staff had been called on duty with safeguard measures. The workers from off stations were directed to join after one week of quarantine period to inspect the appearance of any symptom of COVID-19.
During the second wave of coronavirus (Dec. 2020 to Jan 2021), workforce was again reduced to 50 %. However, during the third and fourth wave, INOR worked with full staff observing all preventive measures. To further reduce the susceptible exposure of staff, hospital follow-up had been transformed to the telephone follow-up where possible.
Different studies on effectiveness of vaccination against COVID spread have reported, a reduction of about 40 to 80 % in the transmission of different corona variants for a range of commercially available vaccines [18-22]. Booster dose of vaccine can further reduce the risk of covid contraction down to 89% [23, 24]. In this view, early vaccination of the whole staff of INOR has been encouraged to minimize the chance of contracting coronavirus. As of now, 100 % staff of INOR has been fully vaccinated while >95 % staff has received booster dose too.
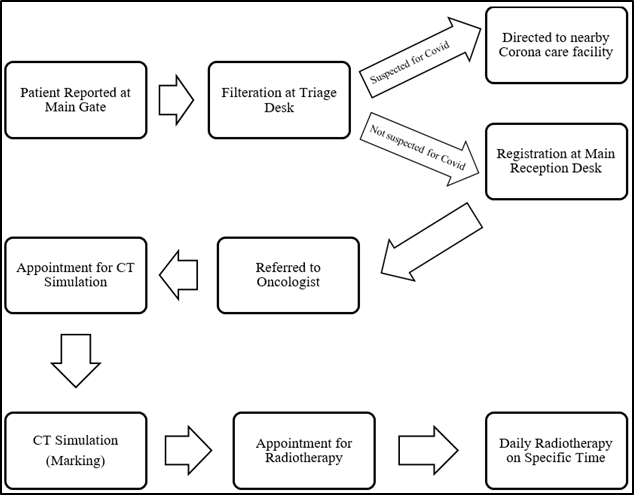
Establishment of Triage center
Establishment of triage center for filtration of COVID suspected patients can effectively reduce the probability of corona virus transmission and cause safer diversion of Covid patients to specific hospital department [25, 26]. INOR has also followed the policy of not entertaining the COVID-19 to minimize the probability of virus spread to other patients and hospital staff. In this regard, a triage facility (for sorting out and classification of patients to determine the priority of need and place of treatment) has been established where the suspected patients and/or their attendants were segregated. The suspected patients were filtered and scored for likelihood of carrying the infection on the basis of their contact history and appearance of COVID-19 symptoms (triage filtration form developed for segregation is given at appendix A). In case the patient score was more than the pre-set value, he/she used to be referred to nearby designated corona care center.
Amendments in Patients Reception / Waiting Areas / route of entry
In order to maintain the social distancing for patients and their attendants, the following amendments have been made in reception and waiting areas of INOR, being the most crowded places.
- Before forwarding to the reception desk in main building, all the patients with their attendants have been directed to a triage section that has been established outside the main (covered) building at the main gate. All the patients used to visit their respective triage desk (segregated as radiotherapy, chemotherapy and other diagnostic facilities) and if filtered for being not suspected for COVID-19, they would wait for their turn outside the main building to get entertained.
- Waiting areas have also been shifted and extended outside the main building of hospital. Only 2-3 patients used to be called and let to wait in the waiting areas of respective departments.
The entry route for radiotherapy patients has been specified to minimize the contact as shown in Figure 2. The crowding is avoided at each point of this route to maintain social distancing.
Figure 2. Flow diagram showing the entry route of radiotherapy patients. If found suspected for COVID-19 at triage centre, patients are referred to the nearby designated corona care centre. Appointment for simulation and radiotherapy is given considering to avoid crowding.
Regarding the awareness of patients and their attendants, posters/placard with precautionary measures against COVID-19 to be taken during their hospital visit and thereafter, have been displayed. Furthermore, the updated recommendations are being issued to workers time to time for their safety from the coronavirus and also to provide guidelines to be followed in case the infection is contracted.
Miscellaneous Measures
Additionally, the following safeguard measures have been taken to minimize the transmission of infection to the workers and patients.
- Adopting the policy of one attendant per patient
- Compulsion on using face masks in hospital premises
- Employing non-contact IR thermal scanners for triage filtration of patients
- Provision of sanitizer to all employees and making them readily available at different places
- Provision of PPEs to workers
- Frequent disinfecting of equipment and the places
- Cessation of biometric attendance of employees
The preventive measures taken against COVID-19 at INOR are summarized in Table 1.
Table 1. Summary of preventive measures adopted at INOR against Covid-19
|
Preventive Measures |
Detail |
||
|
Hypofractionated protocol for radiation therapy of cancer patients [10] |
· Reduced number of patients visits at hospital |
|
|
|
Ventilation [11] |
· Installation of high power exhaust fans · Windows opening · Shifting patients waiting areas from covered area of hospital building to open air. |
|
|
|
Physical Distancing [12] |
· Modification in seating arrangement of patients · Managing time and distance for patients queues · Converting physical meetings and seminars to online meetings/seminars · Installing transparent boundary around Physician’s desk for patients’ consultation. · Increasing number of entrance and exit gates |
|
|
|
PPEs [17] |
· Provision of masks, respirators gowns, shoe covers and head covers · Wearing double mask |
|
|
|
Hand Hygiene [13] |
· Provision of hand sanitizers at different places · Signage placing to remind frequent hand washing · Ceasing biometric attendance (with thumb) |
|
|
|
Disinfection of equipment and environmental surfaces [14-16] |
· Bleach solution for surfaces and floor mopping · 80% alcohol for equipment disinfection |
|
|
|
Establishing Triage center [26] |
· To filter out COVID suspected patients and visitors |
|
|
|
· 100 % employees are vaccinated |
|
||
Impact of COVID-19 on INOR from different aspects
The preventive measures taken against COVID-19 has significantly reduced the impact of Covid-19 on INOR. An overall reduced impact is observed in successive waves compared to previous one. Detail is given as under.
Patient Flux
During the first wave, the patients flux fell down tremendously owing to lock down situation, closure of guest houses/hotels and public transport hindering the patients from far flung areas. Lack of resources, particularly in lock down situation, has also been a cause to reduced patients’ visits. Cessation of allied cancer care services, mainly diagnostic services, could also be a reason of decreased number of new patients. Considering the limited budget, confusion in handling the COVID-19 situation, lacking the standard operating procedures for patient handling and deficiency of PPEs for staff during the first wave of epidemic in Pakistan, a policy decision was made to delay the radiotherapy of new patients, except for those requiring a single fraction with palliative setup. While the patients who were already receiving radiotherapy were let to complete the remaining fractions. Among these, few were converted to hypofractionated protocol, on case to case basis, for early completion of their course. Hypofractionation protocol of 40.5 Gy in 15 fractions (over 3 weeks period) was implemented which has been reported to result in equivalent disease control and improved late and acute toxicity compared to standard fractionation of 50 Gy in 25 fractions over the period of 5 weeks [27-29]. The bar chart shown in Figure 1 shows the fall in patient flux during the first wave of the pandemic (April - July 2020). A surge in patient number is seen in June 2020, after lifting the lock-down situation and modified policy decision of catering all new patients with preventive measures.
During the second (Nov. 2020 to Feb. 2021), third (Apr. to Jun. 2021) and fourth (Jul. to Oct. 2021) wave, of the pandemic, drop in patients flux is less pronounced due to preventive measures taken at INOR against COVID.
It is noteworthy here that usually a significant rise in patient number during spring and summer season (from March onwards) has been seen in previous years due to favorable weather condition in this region. This factor also needs consideration while comparing patient data with winter months (December to February).

Figure 3. Number of new patients who received radiotherapy at INOR from December 2019 to December 2021. Duration of four waves of coronavirus is indicated at the top [30].
Impact on quality assurance and personal dosimetry services
The routine quality assurance program of radiotherapy department has not been impacted much. After proper cleaning and disinfection of equipment, Daily/monthly quality control test of equipment have been carried out as per planned schedule. However, annual beam output measurement of Co-60 unit from secondary standard dosimetry lab (SSDL) Islamabad, that was due in April 2020, was postponed to February 2021 due to closure of SSDL services. In addition to existing pre-treatment quality assurance procedures of radiotherapy equipment, extensive disinfecting procedures have been implemented that has additionally burdened the labour of employees as well have caused a sense of fear/anxiety for the risk of contracting the infection.
COVID-19 pandemic has also left an impact on the personal dosimetry of radiation workers of INOR. Routinely personal dosimeters (TLDs) are read on quarterly basis from our central TLD reading facility, Radiation Dosimetry Group, Islamabad. However, owing to the cessation of their services, TLD reading has been postponed for about two quarters during this pandemic in the first wave. Whereas it remained as per routine thereafter after following preventive measures. The personal radiation dose of radiotherapy staff reduced considerably during Covid that may be ascribed to treating less number of patients on Cobalt-60 teletherapy machine. For instance, the average radiation dose of staff working in radiotherapy department was found 0.03 mSv/month during first Covid wave compared to 0.16 mSv/month during pre-Covid quarter. Another possible reason of rendering low dose record of workers could be the fading of thermoluminescent signal (that is directly proportional to radiation absorbed dose) due to delay in TLD reading [31].
Impact on the installation of new equipment
INOR has recently extended its radiotherapy facilities and installed new Linear accelerator (LINAC) recently. The base plate of new LINAC was installed in December 2019, and the civil work of bunker was completed in March 2021. The next phase of installation and acceptance of LINAC and dosimetry system by two different foreign engineers was due in April 2020. It was anticipated that commissioning of LINAC would be completed by the end of July 2020 following by the installation / commissioning of treatment planning system. Whereas the treatment of patients with new LINAC was expected to be started in the last quarter of 2020. However, due to the halting of international flights and reluctance of foreign experts to visit during this pandemic, the planned schedule altered altogether. Installation and acceptance of LINAC was delayed till December 2020 followed by acceptance of dosimetry system in February 2021. Commissioning of LINAC was performed in March 2021 following all preventive measures. Patients’ treatment on new LINAC has been started since April 2021.
Financial Impact
A significant negative financial impact has been observed on INOR budget since the onset of COVID-19 pandemic. Till now, INOR has spent more than 1 million PKR on the purchase of PPEs and other related items since late March 2020. While much of the commodities of significant worth have been received as donations from National Disaster Management Authority and PAEC headquarters. Recurring expenditures on the regular supplies of INOR like disinfecting items, sanitizers, masks, gloves etc. has also been increased to many folds. Contrarily, revenue of INOR was reduced to about 30 % during the first wave of the emergency. However, it returned to normal after that owing to the extensive measures taken to fight against COVID.
Conclusion
In conclusion, coronavirus has affected the cancer care services and transformed almost the every aspect of the facility ultimately causing a significant financial burden on INOR in the first wave of COVID-19. However owing to the stringent and timely measures, the negative impact of Covid has been reduced remarkably. The ratio of contracting coronavirus among the employees of INOR has been found very low (<10 %) during this whole pandemic and no mortality has been reported so far. In each subsequent wave of coronavirus, its impact on routine working of INOR radiotherapy department has been reduced due to wise policy decisions for improving preventive measures based on experiences in previous waves. The 100 % staff has been fully vaccinated till date. Owing to these measures, No mortality has been reported so far due to covid-19 in INOR employees. Being a low budget hospital, INOR has taken the measures against COVID-19 optimally for continuation of its cancer care services smoothly as well as to reduce its financial impact on the resources. Adopting the suggested measures, the uninterrupted radiotherapy services to cancer patients can be provided with minimal probability of transmission of the corona virus.
REFRENCES
[1] WHO. (July 1). Coronavirus disease (COVID-19) pandemic, World Health Organization (WHO). Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019-coronavirus-2019
[2] NCOC. (July 1). CORONAVIRUS IN PAKISTAN, National Command and Operation Center (NCOC), Pakistan. Available: www.covid.gov.pk
[3] R. Redfield, "CDC Director On Models For The Months To Come: 'This Virus Is Going To Be With Us'," ed, March 11, 2020.
[4] F. P. Lyngse, L. H. Mortensen, M. J. Denwood, L. E. Christiansen, C. H. Møller, R. L. Skov, et al., "SARS-CoV-2 Omicron VOC Transmission in Danish Households," medRxiv, 2021.
[5] S. Mayor, "COVID-19: impact on cancer workforce and delivery of care," The Lancet Oncology, vol. 21, p. 633, 2020.
[6] N. M. Kuderer, T. K. Choueiri, D. P. Shah, Y. Shyr, S. M. Rubinstein, D. R. Rivera, et al., "Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study," The Lancet, 2020.
[7] W. Liang, W. Guan, R. Chen, W. Wang, J. Li, K. Xu, et al., "Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China," The Lancet Oncology, vol. 21, pp. 335-337, 2020.
[8] L. Y. Lee, J. B. Cazier, T. Starkey, C. Turnbull, U. C. C. M. P. Team, R. Kerr, et al., "COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study," The Lancet, 2020.
[9] H. Nagar and S. C. Formenti, "Cancer and COVID-19—potentially deleterious effects of delaying radiotherapy," Nature Reviews Clinical Oncology, vol. 17, pp. 332-334, 2020.
[10] C. Coles, C. Aristei, J. Bliss, L. Boersma, A. Brunt, S. Chatterjee, et al., "International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic," Clinical Oncology, vol. 32, pp. 279-281, 2020.
[11] T. Lipinski, D. Ahmad, N. Serey, and H. Jouhara, "Review of ventilation strategies to reduce the risk of disease transmission in high occupancy buildings," International Journal of Thermofluids, vol. 7, p. 100045, 2020.
[12] W. C. Koh, L. Naing, and J. Wong, "Estimating the impact of physical distancing measures in containing COVID-19: an empirical analysis," International Journal of Infectious Diseases, vol. 100, pp. 42-49, 2020.
[13] G. Cavanagh and C. G. Wambier, "Rational hand hygiene during the coronavirus 2019 (COVID-19) pandemic," Journal of the American Academy of Dermatology, vol. 82, p. e211, 2020.
[14] W. H. Organization, "Water, sanitation, hygiene and waste management for COVID-19: technical brief, 03 March 2020," World Health Organization2020.
[15] W. H. Organization, "Cleaning and disinfection of environmental surfaces in the context of COVID-19," 2020.
[16] L. Cirrincione, F. Plescia, C. Ledda, V. Rapisarda, D. Martorana, R. E. Moldovan, et al., "COVID-19 pandemic: Prevention and protection measures to be adopted at the workplace," Sustainability, vol. 12, p. 3603, 2020.
[17] S. H. Park, "Personal protective equipment for healthcare workers during the COVID-19 pandemic," Infection & chemotherapy, vol. 52, p. 165, 2020.
[18] R. J. Harris, J. A. Hall, A. Zaidi, N. J. Andrews, J. K. Dunbar, and G. Dabrera, "Effect of vaccination on household transmission of SARS-CoV-2 in England," New England Journal of Medicine, vol. 385, pp. 759-760, 2021.
[19] A. S. Shah, C. Gribben, J. Bishop, P. Hanlon, D. Caldwell, R. Wood, et al., "Effect of vaccination on transmission of SARS-CoV-2," New England Journal of Medicine, vol. 385, pp. 1718-1720, 2021.
[20] D. W. Eyre, D. Taylor, M. Purver, D. Chapman, T. Fowler, K. Pouwels, et al., "The impact of SARS-CoV-2 vaccination on Alpha and Delta variant transmission," Medrxiv, 2021.
[21] K. K. Riemersma, B. E. Grogan, A. Kita-Yarbro, G. E. Jeppson, D. H. O’Connor, T. C. Friedrich, et al., "Vaccinated and unvaccinated individuals have similar viral loads in communities with a high prevalence of the SARS-CoV-2 delta variant," MedRxiv, 2021.
[22] F. Lyngse, L. Mortensen, and M. Denwood, "SARS-CoV-2 Omicron VOC transmission in Danish households. medRxiv," ed: Posted December, 2021.
[23] C. Stokel-Walker, "What do we know about covid vaccines and preventing transmission?," bmj, vol. 376, 2022.
[24] R. R. ASSESSMENT, "Assessment of the further spread and potential impact of the SARS-CoV-2 Omicron variant of concern in the EU/EEA, 19th update," 2022.
[25] A. Gilbert, E. Brasseur, M. Petit, A. F. Donneau, A. Diep, S. Hetzel Campbell, et al., "Immersion in an emergency department triage center during the Covid-19 outbreak: first report of the Liège University hospital experience," Acta Clinica Belgica, pp. 1-7, 2020.
[26] N. NeJhaddadgar, A. Ziapour, G. Zakkipour, J. Abbas, M. Abolfathi, and M. Shabani, "Effectiveness of telephone-based screening and triage during COVID-19 outbreak in the promoted primary healthcare system: a case study in Ardabil province, Iran," Journal of Public Health, pp. 1-6, 2020.
[27] A. Gupta, N. Ohri, and B. G. Haffty, "Hypofractionated radiation treatment in the management of breast cancer," Expert review of anticancer therapy, vol. 18, pp. 793-803, 2018.
[28] E. Ippolito, C. G. Rinaldi, S. Silipigni, C. Greco, M. Fiore, A. Sicilia, et al., "Hypofractionated radiotherapy with concomitant boost for breast cancer: a dose escalation study," The British Journal of Radiology, vol. 92, p. 20180169, 2019.
[29] F. Shaikh, J. Chew, T. Hochman, J. Purswani, O. Maisonet, E. Peat, et al., "Hypofractionated whole-breast irradiation in women less than 50 years old treated on 4 prospective protocols," International Journal of Radiation Oncology* Biology* Physics, vol. 101, pp. 1159-1167, 2018.
[30] "COVID-19 Results Briefing," Institute for Health Metrics and Evaluation (IHME), Univerity of Washington USA. https://www.healthdata.org/sites/default/files/files/Projects/COVID/2022/165_briefing_Pakistan.pdf 13 January 2022 January 2022.
[31] Y. Lee, Y. Won, and K. Kang, "A method to minimise the fading effects of LiF: Mg, Ti (TLD-600 and TLD-700) using a pre-heat technique," Radiation Protection Dosimetry, vol. 164, pp. 449-455, 2015.
Appendix A: Supplementary Data
Patients visiting INOR, are assessed on the basis of the criteria described in the following form required to be filled at the triage center.
|
INOR TRIAGE FILTRATION FORM Date:_________
Hand Washed (YES/NO):________Hand Sanitized (YES/NO):_______Masked (YES/NO):_________
Patient’s Details & Travel/ Contact History-(Sindh, GB, Peshawar, abroad etc. & COVID-19 Contact)
Attendant(s) Details & Travel/Contact History-(Sindh, GB, Peshawar, abroad etc. & COVID-19 Contact)
Symptoms/Signs
Entry Allowed :(YES/NO):_______Number of Persons (Patient + Attendants): __________
Duty Person- Name:____________________PIN___________Sig:_______
Focal Person for COVID-19 (For final decision of allowing the entry in hospital)
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||