Synthesis and Characterization of Silver Nanoparticles Conjugated with Folate and Curcumin for Their Anti-Cancer Activity
Keywords:
Silver nanoparticles (Ag NPs), Polyethylene Glycol (PEG), Chemotherapy, Cancer, Targeted Drug DeliveryAbstract
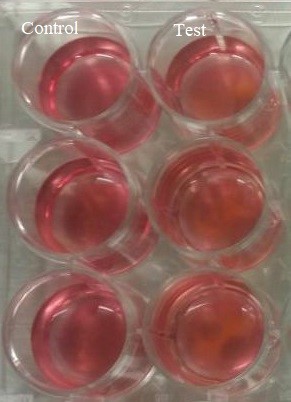
Nanoparticles are small particles with sizes ranging from 1 to 100 nanometers. Silver nanoparticles, composed of silver at the nanoscale, have been widely used in various fields including medicine, healthcare, food, and commercial industries. While silver nanoparticles can be harmful to normal cells depending on their concentration and exposure time, they are highly effective for wound healing and antibacterial applications. Historically, silver was used as a natural antibiotic. In this study, silver nanoparticles were conjugated with curcumin and folic acid using the glutaraldehyde method due to their anti-cancer properties. Curcumin is known for its ability to kill cancer cells, while folic acid—an organic form of vitamin B9—helps in the creation and preservation of healthy cells. The silver nanoparticles were first modified with polyethylene glycol (PEG), then conjugated with curcumin and folic acid. Curcumin was attached through the NH2 group, and folic acid was linked via the carbonyl group, both through PEG. The average crystalline size was calculated using X-ray diffraction (XRD), and functional groups were identified using Fourier-transform infrared spectroscopy (FTIR). These silver nanoparticles are considered to be more beneficial and less harmful than traditional chemotherapy or radiotherapy for targeting and destroying tumor cells.
References
G. E.-S. B. & A. A. Olabode Omotoso, John Oluwafemi Teibo, Festus Adebayo Atiba, Tolulope Oladimeji, Oluwatomiwa Kehinde Paimo, Farid S. Ataya, “Addressing cancer care inequities in sub-Saharan Africa: current challenges and proposed solutions,” Int. J. Equity Health, vol. 22, no. 189, 2023, doi: https://doi.org/10.1186/s12939-023-01962-y.
J. A. Siegel RL, Miller KD, Fuchs HE, “Cancer statistics,” Cancer J Clin, vol. 72, no. 1, 2022, [Online]. Available: https://www.cancer.gov/about-cancer/understanding/statistics
J. A. & A. N. Aasma Zafar, Summaiya Khatoon, Muhammad Jawad Khan, “Advancements and limitations in traditional anti-cancer therapies: a comprehensive review of surgery, chemotherapy, radiation therapy, and hormonal therapy,” Discov. Oncol., vol. 16, no. 607, 2025, doi: https://doi.org/10.1007/s12672-025-02198-8.
P. S. C. Prof Christian Pfister, Gwenaelle Gravis, Aude Flechon, Christine Chevreau, Hakim Mahammedi, Brigitte Laguerre, Aline Guillot, Prof Florence Joly, Prof Michel Soulie, Prof Yves Allory, Valentin Harter, “Perioperative dose-dense methotrexate, vinblastine, doxorubicin, and cisplatin in muscle-invasive bladder cancer (VESPER): survival endpoints at 5 years in an open-label, randomised, phase 3 study,” Lancet Oncol., vol. 25, no. 2, pp. 255–264, 2024, doi: https://doi.org/10.1016/S1470-2045(23)00587-9.
C. M. V. & S. G. B. Ada Radu, Delia Mirela Tit, Laura Maria Endres, Andrei-Flavius Radu, “Naturally derived bioactive compounds as precision modulators of immune and inflammatory mechanisms in psoriatic conditions,” Inflammopharmacology, vol. 33, pp. 527–549, 2025, doi: https://doi.org/10.1007/s10787-024-01602-z.
J. Z. & Y. S. Huning Jiang, Jiahua Cui, Hao Chu, Tingting Xu, Mengyan Xie, Xinming Jing, Jiali Xu, “Targeting IL8 as a sequential therapy strategy to overcome chemotherapy resistance in advanced gastric cancer,” Cell Death Discov., vol. 8, no. 235, 2022, doi: https://doi.org/10.1038/s41420-022-01033-1.
G. T. Peter Takáč, Radka Michalková, Martina Čižmáriková, Zdenka Bedlovičová, Ľudmila Balážová, “The Role of Silver Nanoparticles in the Diagnosis and Treatment of Cancer: Are There Any Perspectives for the Future?,” Life, vol. 13, no. 2, p. 466, 2023, doi: https://doi.org/10.3390/life13020466.
M. E. & A. A. Soha Gomaa, Mohamed Nassef, Ahlam Abu-Shafey, “Impacts of loading thymoquinone to gold or silver nanoparticles on the efficacy of anti-tumor treatments in breast cancer with or without chemotherapeutic cisplatin,” BMC Biotechnol., vol. 25, no. 26, 2025, doi: https://doi.org/10.1186/s12896-025-00958-6.
M. I. Muhammad Sarfraz, Abida Khan, Gaber El-Saber Batiha, Ammara Saleem, Basiru Olaitan Ajiboye, Mehnaz Kamal, Abuzer Ali, Nawaf M. Alotaibi, Shams Aaghaz, Muhammad Irfan Siddique, “Nanotechnology-Based Drug Delivery Approaches of Mangiferin: Promises, Reality and Challenges in Cancer Chemotherapy,” Cancers (Basel)., vol. 15, no. 16, p. 4194, 2023, doi: https://doi.org/10.3390/cancers15164194.
George Pasparakis, “Recent developments in the use of gold and silver nanoparticles in biomedicine,” Wiley Interdiscip Rev Nanomed Nanobiotechnol, vol. 14, no. 5, p. e1817, 2022, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/35775611/
N. Sakshi Sehgal, Jagdeep Kumar, “Involvement of gold and silver nanoparticles in lung cancer nanomedicines: A review,” Mater. proceeding, vol. 62, no. 12, pp. 6468–6476, 2022, doi: https://doi.org/10.1016/j.matpr.2022.04.199.
S. Palazzolo et al., “The Clinical Translation of Organic Nanomaterials for Cancer Therapy: A Focus on Polymeric Nanoparticles, Micelles, Liposomes and Exosomes,” Curr. Med. Chem., vol. 25, no. 34, pp. 4224–4268, Sep. 2017, doi: 10.2174/0929867324666170830113755.
L. Z. Bingqian Li, Huili Shao, Lei Gao, Huan Li, Huagang Sheng, “Nano-drug co-delivery system of natural active ingredients and chemotherapy drugs for cancer treatment: a review,” Drug Deliv., vol. 29, no. 1, pp. 2130–2161, 2022, doi: https://doi.org/10.1080/10717544.2022.2094498.
F. S. & H. K. A. Nima Beheshtizadeh, Zahra Amiri, Seyedeh Zoha Tabatabaei, Amir Abbas Seraji, Maliheh Gharibshahian, Akram Nadi, Morvarid Saeinasab, “Boosting antitumor efficacy using docetaxel-loaded nanoplatforms: from cancer therapy to regenerative medicine approaches,” J. Transl. Med. Vol., vol. 22, no. 520, 2024, doi: https://doi.org/10.1186/s12967-024-05347-9.
M. S. A. Azeez Yusuf, Awatif Rashed Z. Almotairy, Hanan Henidi, Ohoud Y. Alshehri, “Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems,” Polymers (Basel)., vol. 15, no. 7, p. 1596, 2023, doi: https://doi.org/10.3390/polym15071596.
S. S. H. S. and B. Z. R. Shazina Jabeen, Rahmatullah Qureshi, Mehmooda Munazir, Muhammad Maqsood, Mubashrah Munir, “Application of green synthesized silver nanoparticles in cancer treatment—a critical review,” Mater. Res. Express, vol. 8, no. 9, p. 092001, 2021, doi: 10.1088/2053-1591/ac1de3.
R. R. Miranda, I. Sampaio, and V. Zucolotto, “Exploring silver nanoparticles for cancer therapy and diagnosis,” Colloids Surfaces B Biointerfaces, vol. 210, p. 112254, 2022, doi: https://doi.org/10.1016/j.colsurfb.2021.112254.
M. R. D. Dhanunjaya Kumar Chadive, Priyanka Gurrala, “Biogenic synthesis of silver nanoparticles from the leaf extract of Erythroxylum Monogynum Roxb: Evaluation of antibacterial and anticancer effects,” Nano-Structures & Nano-Objects, vol. 39, p. 101222, 2024, doi: https://doi.org/10.1016/j.nanoso.2024.101222.
D. A. E. M. A. Sumera Zaib, Hamid Saeed Shah, Imtiaz Khan, Zobia Jawad, Muhammad Sarfraz, Huma Riaz, Hafiz Muhammad Mazhar Asjad, Memoona Ishtiaq, Hanan A. Ogaly, Gehan Othman, “Fabrication and evaluation of anticancer potential of diosgenin incorporated chitosan-silver nanoparticles; in vitro, in silico and in vivo studies,” Int. J. Biol. Macromol., vol. 254, no. 3, p. 127975, 2024, doi: https://doi.org/10.1016/j.ijbiomac.2023.127975.
S. S. T.S. Saranya, V.K. Rajan, Raja Biswas, R. Jayakumar, “Synthesis, characterisation and biomedical applications of curcumin conjugated chitosan microspheres,” Int. J. Biol. Macromol., vol. 110, pp. 227–233, 2018, doi: https://doi.org/10.1016/j.ijbiomac.2017.12.044.
C.-Y. A. & H.-F. J. Liang Shen, Cui-Cui Liu, “How does curcumin work with poor bioavailability? Clues from experimental and theoretical studies,” Sci. Rep., vol. 6, p. 20872, 2016, doi: https://doi.org/10.1038/srep20872.
Ali Ubeyitogullari & Ozan N. Ciftci, “A novel and green nanoparticle formation approach to forming low-crystallinity curcumin nanoparticles to improve curcumin’s bioaccessibility,” Sci. Rep., vol. 9, no. 19112, 2019, doi: https://doi.org/10.1038/s41598-019-55619-4.
S. W. Shuting Chen, Jie Wu, Qiang Tang, Chenlan Xu, Yan Huang, Da Huang, Fang Luo, Yuanzi Wu, Fen Yan, Zuquan Weng, “Nano-micelles based on hydroxyethyl starch-curcumin conjugates for improved stability, antioxidant and anticancer activity of curcumin,” Carbohydr. Polym., vol. 228, p. 115398, 2020, doi: https://doi.org/10.1016/j.carbpol.2019.115398.
G. Dhulappanavar et al., “Characterization of silver nanoparticles biosynthesized using lemon juice,” Proc. Int. Conf. Nanosci. Eng. Technol. ICONSET 2011, pp. 258–262, 2011, doi: 10.1109/ICONSET.2011.6167936.
A. M. Abdellah, M. A. Sliem, M. Bakr, and R. M. Amin, “Green Synthesis and Biological Activity of Silver–Curcumin Nanoconjugates,” Future Med. Chem., vol. 10, no. 22, pp. 2577–2588, Nov. 2018, doi: 10.4155/FMC-2018-0152.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 50sea

This work is licensed under a Creative Commons Attribution 4.0 International License.