Barriers to Maternal Health Care Accessibility and Its Causal Determinants in Faisalabad, Pakistan: A Geospatial Assessment
Keywords:
Maternal Health Care, Geospatial Accessibility, Maternal Mortality, Determinants, PakistanAbstract
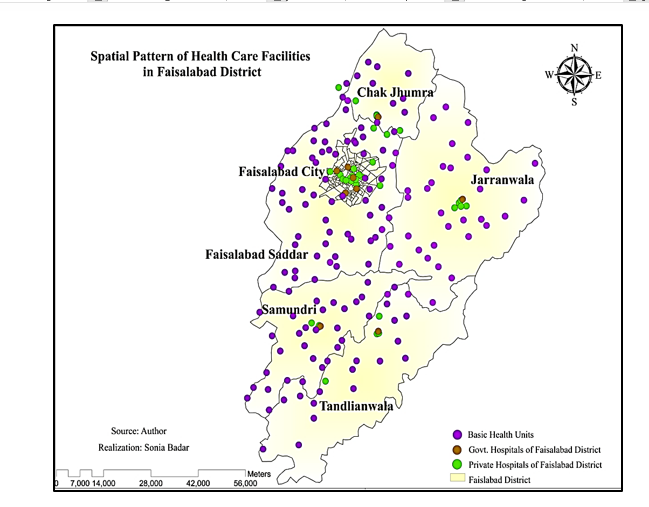
Access to maternal healthcare is a critical determinant of maternal and neonatal health outcomes, yet it remains a neglected issue in many developing regions, including Pakistan. This study investigates the spatial distribution and accessibility of maternal healthcare facilities in Faisalabad District using Geographic Information System (GIS) techniques, including point distance analysis and multiple ring buffer analysis. A total of 230 female respondents from six tehsils were surveyed using a structured questionnaire, with data gathered from two major public hospitals in the district. There are 155 Basic Health Units (BHUs) operating within Faisalabad District. 45.2% of respondents reported good accessibility to maternal health facilities, while 43% reported bad and 11.7% worse access. The highest concentration of cases (78 respondents) was within 6–10 km of a health facility. The findings reveal significant spatial disparities in access to healthcare facilities, particularly in rural and peripheral areas such as Tandlianwala, Chak Jhumra, and Samundri. Many women reside more than 20 kilometers from the nearest well-equipped hospital, and road conditions—ranging from poor to non-existent—further limit physical accessibility. The multiple ring buffer analysis demonstrates that several remote settlements fall outside the 12-mile buffer, indicating critical service gaps. Additionally, economic constraints and lack of public transportation exacerbate the situation, limiting women's ability to seek timely antenatal care. The overcrowding of urban public hospitals and the high cost and low quality of private healthcare further restrict options for low-income groups. The study underscores the urgent need for decentralized planning, infrastructure improvement, and equitable distribution of maternal health services, especially in underserved rural regions.
References
WHO, “Maternal Health.” Accessed: Sep. 17, 2025. [Online]. Available: www.who.int/health-topics/maternal-health#tab=tab_1
IS GLOBAL, “Research, Maternal, Child and Reproductive Health Maternal, Child and Reproductive Health,” 2022, [Online]. Available: https://www.isglobal.org/en/maternal-child-reproductive
B. G. Sanni Yaya, “Global Inequality in Maternal Health Care Service Utilization: Implications for Sustainable Development Goals,” Heal. Equity, vol. 3, no. 1, pp. 145–154, 2019, doi: 10.1089/heq.2018.0082.
M. C. Hogan et al., “Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5,” Lancet, vol. 375, no. 9726, pp. 1609–1623, May 2010, doi: 10.1016/S0140-6736(10)60518-1.
National Institute of Population Studies (NIPS) [Pakistan] and ICF, “PAKISTAN DEMOGRAPHIC AND HEALTH SURVEY 2017-18,” 2019, [Online]. Available: https://dhsprogram.com/pubs/pdf/FR354/FR354.pdf
National Institute of Population Studies and P. Islamabad, “Demographic and Health Survey 2006-07,” Macro International Inc. Calverton, Maryland USA. Accessed: Sep. 01, 2025. [Online]. Available: https://dhsprogram.com/pubs/pdf/fr200/fr200.pdf
National Institute of Population Studies (NIPS) [Pakistan] and ICF, “Pakistan Maternal Mortality Survey,” 2020, [Online]. Available: https://dhsprogram.com/pubs/pdf/PR128/PR128.pdf
M. Mustafa, A. Batool, B. Fatima, F. Nawaz, K. Toyama, and A. A. Raza, “Patriarchy, Maternal Health and Spiritual Healing: Designing Maternal Health Interventions in Pakistan,” Conf. Hum. Factors Comput. Syst. - Proc., Apr. 2020, doi: 10.1145/3313831.3376294/SUPPL_FILE/A167-MUSTAFA-PRESENTATION.MP4.
L. S. Richard Vergunst, “’You must carry your wheelchair’--barriers to accessing healthcare in a South African rural area,” Glob. Health Action, vol. 8, no. 1, 2015, doi: 10.3402/gha.v8.29003.
W. Luo and F. Wang, “Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region,” Environ. Plan. B Plan. Des., vol. 30, no. 6, pp. 865–884, 2003, doi: 10.1068/B29120,.
S.-U.-Z. Jabeen, S., Zaman, B. S., Ahmed, A., & Bhatti, “Maternal mortality,” Prof. Med. J., vol. 17, no. 4, 2010, [Online]. Available: https://www.researchgate.net/publication/49616040_MATERNAL_MORTALITY
K. J. João Paulo Souza, Louise Tina Day, Ana Clara Rezende-Gomes, Jun Zhang, Rintaro Mori, Adama Baguiya, “A global analysis of the determinants of maternal health and transitions in maternal mortality,” Lancet Glob Heal., 2024, doi: 10.1016/S2214-109X(23)00468-0.
GOP, “PRSP Budgetary Expenditures, Finance Division,” 2024, [Online]. Available: https://www.finance.gov.pk/poverty/PRSP_Expenditure_FY_2022_23.pdf
GOP, “PAKISTAN ECONOMIC SURVEY 2023-24,” | Ministry of Finance | Government of Pakistan |. Accessed: Sep. 01, 2025. [Online]. Available: https://finance.gov.pk/survey_2024.html
“Maternal Mortality in Pakistan - The Borgen Project.” Accessed: Sep. 17, 2025. [Online]. Available: https://borgenproject.org/maternal-mortality-pakistan/
M. Sarkar, T. B. Roy, and R. Roy, “An Assessment Study on Hierarchical Integrity of Road Connectivity and Nodal Accessibility of Maternal Health Care Service Centres in Itahar Block, Uttar Dinajpur District, West Bengal,” pp. 439–457, 2022, doi: 10.1007/978-981-16-7310-8_22.
N. Shah, R. Sultan, and N. Siddiqui, “Social Determinants of Maternal Mortality: A qualitative study in Balochistan,” J. LAW, Soc. Manag. Sci., vol. 2, no. 2, pp. 144–151, Dec. 2023, Accessed: Sep. 02, 2025. [Online]. Available: https://jlsms.org/index.php/jlsms/article/view/38
Pakistan Bureau os statics, “7th Population & Housing Census ‘First Ever Digital Census’, Key Findings Report,The Largest Digitization Exercise of South Asia,” 2023, [Online]. Available: https://www.pbs.gov.pk/sites/default/files/population/2023/Key_Findings_Report.pdf
S. T. R. Sarwat Ara, “Maternal mortality in Faisalabad and Millennium Developmental Goals,” Pakistan Journal of Medical Sciences Online. Accessed: Sep. 01, 2025. [Online]. Available: https://www.researchgate.net/publication/288106362_Maternal_mortality_in_Faisalabad_and_Millennium_Developmental_Goals
A. Arif et al., “Maternal and Perinatal Death Surveillance and Response in Balochistan, Pakistan - Causes & Contributory Factors of Maternal Deaths,” J. Gynecol. Obstet. 2022, Vol. 10, Page 1, vol. 10, no. 1, pp. 1–5, Jan. 2022, doi: 10.11648/J.JGO.20221001.11.
M. Hanif et al., “Maternal Mortality in Rural Areas of Pakistan: Challenges and Prospects,” Rural Heal., Jun. 2021, doi: 10.5772/INTECHOPEN.96934.
A. Khan, V. Izhar, and M. A. Viqar, “MATERNAL MORBIDITY AND MORTALITY IN PAKISTAN - AN OVERVIEW OF MAJOR CONTRIBUTORS: Maternal Morbidity And Mortality,” Pakistan Armed Forces Med. J., vol. 67, no. 4, pp. 635–40, Aug. 2017, Accessed: Sep. 17, 2025. [Online]. Available: https://www.pafmj.org/PAFMJ/article/view/741
R. Mehboob, F. J. Ahmad, S. A. Gilani, A. Hassan, S. Khalid, and J. Akram, “Maternal Mortality Ratio in Low Income Developing Countries-Focusing on Pakistan,” Jun. 2020, doi: 10.20944/PREPRINTS202006.0354.V1.
R. Mehboob et al., “Maternal Mortality Ratio in Low Income Developing Countries,” Glob. Women’s Heal., Feb. 2021, doi: 10.5772/INTECHOPEN.95258.
S. H. Ali Mohammad Mir, Stephen Pearson, Saleem Shaikh, Mumraiz Khan, Irfan Masud, “Maternal Mortality due to Eclampsia in Khyber Pakhtunkhwa: Identifying Underlying Risk Factors, and Care-seeking Behaviours,” J Pak Med Assoc, vol. 69, no. 7, pp. 934–938, 2019, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/31308557/
S. Naz, M. Aslam, and R. Karim, “Social And Cultural Factors Influencing Maternal Mortality In Khyber Pakhtunkhwa- Pakistan,” J. Posit. Sch. Psychol. , vol. 6, no. 10, pp. 453–465, Oct. 2022, Accessed: Sep. 17, 2025. [Online]. Available: https://journalppw.com/index.php/jpsp/article/view/13063
S. A. Saiqa Noor, Nazia Wahid, Sobia Ali, “Maternal Mortality: A 5-year analysis at a District Headquarter Hospital in Pakistan,” J Ayub Med Coll Abbottabad, pp. S655–S658, 2020, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/33754526/
Sonia Omer, “The Social and Cultural Factors of Maternal Mortality in the Context of Three Delays: The perspective of Lady Health Workers of South Punjab, Pakistan,” Pakistan Vis., vol. 2, no. 1, 2019, [Online]. Available: https://pu.edu.pk/images/journal/studies/PDF-FILES/11_v20_1_19.pdf
S. Omer, R. Zakar, M. Z. Zakar, and F. Fischer, “The influence of social and cultural practices on maternal mortality: a qualitative study from South Punjab, Pakistan,” Reprod. Health, vol. 18, no. 1, pp. 1–12, Dec. 2021, doi: 10.1186/S12978-021-01151-6/TABLES/2.
M. Qadir, “Trends in Maternal Mortality in a Tertiary Care Hospital of Khyber Pakhtunkhwa,” Pakistan J. Med. Heal. Sci., vol. 18, no. 1, pp. 44–46, Feb. 2024, doi: 10.53350/PJMHS0202418144.
S. S. H. Shah, D. A. A. Wassan, and D. K. Wassan, “Sociological Analysis of Maternal Mortality Rate And Early Marriages of Girls in Rural Areas of Hyderabad Division, Sindh,” Grassroots, vol. 52, no. 02, Dec. 2018, Accessed: Sep. 17, 2025. [Online]. Available: https://sujo.usindh.edu.pk/index.php/Grassroots/article/view/48
N. I. Mariyam Sarfraz, Saira Tariq, Saima Hamid, “SOCIAL AND SOCIETAL BARRIERS IN UTILIZATION OF MATERNAL HEALTH CARE SERVICES IN RURAL PUNJAB, PAKISTAN,” J Ayub Med Coll Abbottabad, vol. 27, no. 4, 2015, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/27004336/
National Institute of Population Studies (NIPS) [Pakistan] and ICF International, “Pakistan Demographic and Health Survey 2012-13,” NIPS ICF Int., 2013, [Online]. Available: https://dhsprogram.com/pubs/pdf/fr290/fr290.pdf
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 50sea

This work is licensed under a Creative Commons Attribution 4.0 International License.