Geodemographic assessment of tuberculosis patients using Principal Component Analysis (PCA) in Gujranwala city, Pakistan
Keywords:
Tuberculosis, socioeconomic, Principal Component Analysis, GujranwalaAbstract
Introduction/Importance of the Study: Tuberculosis (TB) is a highly contagious disease caused by the bacterium Mycobacterium tuberculosis. It has persisted for centuries and primarily affects the lungs, spreading through airborne droplets. First identified by Robert Koch in 1882, TB remains a global health challenge. The World Health Organization (WHO) has been actively working to reduce TB incidence worldwide, and their efforts have led to a decline in infection rates over time. TB is closely related to geodemographic factors, which influence its prevalence and distribution.
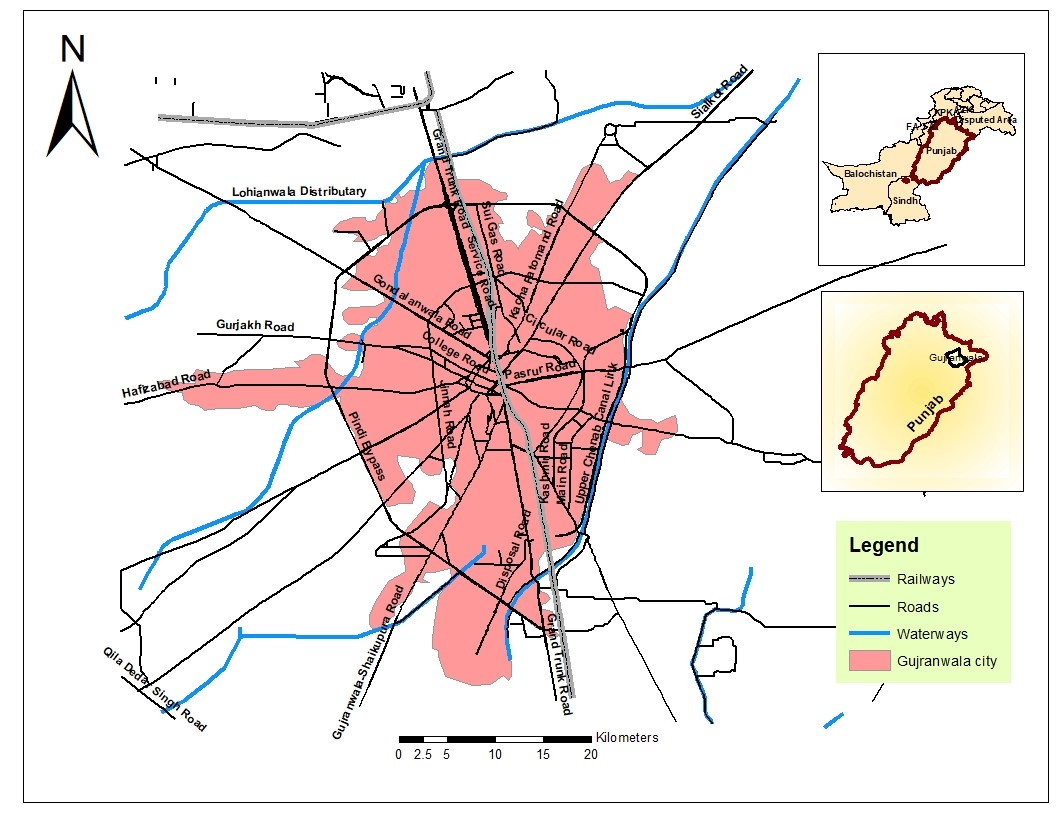
Objective: This study aims to investigate the risk factors, spatial distribution, and hotspot areas of TB in Gujranwala city.
Material and Methods: Primary data were collected through questionnaire surveys, and secondary data were obtained from TB center records. These data were analyzed using statistical Principal Component Analysis (PCA) and Geographic Information System (GIS) software.
Novelty Statement: This study provides a geographical analysis of TB patients, offering significant insights that could enhance TB treatment strategies.
Results and Discussion: The analysis revealed that socioeconomic status, diet, diagnostic practices, and ecological conditions are key risk factors for TB. High-incidence areas are often characterized by poor ecological and economic conditions, predominantly inhabited by low- to middle-income labor class populations. Specific areas such as Ladhewala Wraich, Chicherwali, Kachi Phatuman, and Loyawala face ongoing environmental and socioeconomic challenges.
Concluding Remarks: Addressing these adverse conditions is crucial for reducing TB spread. Strengthening the immune system is also vital in preventing the disease. The government has a critical role in implementing measures to eradicate TB in Pakistan and improve overall public health.
References
C. Zemouri, S. F. Awad, C. M. C. Volgenant, W. Crielaard, A. M. G. A. Laheij, and J. J. de Soet, “Modeling of the Transmission of Coronaviruses, Measles Virus, Influenza Virus, Mycobacterium tuberculosis, and Legionella pneumophila in Dental Clinics,” J. Dent. Res., vol. 99, no. 10, pp. 1192–1198, Sep. 2020, doi: 10.1177/0022034520940288/ASSET/IMAGES/LARGE/10.1177_0022034520940288-FIG1.JPEG.
H. J. Zar and T. W. Ferkol, “The global burden of respiratory disease—Impact on child health,” Pediatr. Pulmonol., vol. 49, no. 5, pp. 430–434, May 2014, doi: 10.1002/PPUL.23030.
K. Floyd, P. Glaziou, A. Zumla, and M. Raviglione, “The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era,” Lancet Respir. Med., vol. 6, no. 4, pp. 299–314, Apr. 2018, doi: 10.1016/S2213-2600(18)30057-2.
G. Sandhu, “Tuberculosis: Current situation, challenges and overview of its control programs in India,” J. Glob. Infect. Dis., vol. 3, no. 2, pp. 143–150, Apr. 2011, doi: 10.4103/0974-777X.81691.
A. Rashid et al., “Ecological footprint of Rawalpindi; Pakistan’s first footprint analysis from urbanization perspective,” J. Clean. Prod., vol. 170, pp. 362–368, Jan. 2018, doi: 10.1016/J.JCLEPRO.2017.09.186.
G. Thornicroft, D. Rose, and A. Kassam, “Discrimination in health care against people with mental illness,” Int. Rev. Psychiatry, vol. 19, no. 2, pp. 113–122, Apr. 2007, doi: 10.1080/09540260701278937.
R. Fatima et al., “Building sustainable operational research capacity in Pakistan: starting with tuberculosis and expanding to other public health problems,” Glob. Health Action, vol. 12, no. 1, Jan. m, doi: 10.1080/16549716.2018.1555215.mia
R. Fatima, “Title: Assessing the burden of missing tuberculosis cases in Pakistan”.
D. C. Ogbuabor and O. E. Onwujekwe, “Governance of tuberculosis control programme in Nigeria,” Infect. Dis. Poverty, vol. 8, no. 1, pp. 1–11, Jun. 2019, doi: 10.1186/S40249-019-0556-2/TABLES/2.
V. Smelov et al., “Rationale and Purpose: The FLUTE Study to Evaluate Fluorography Mass Screening for Tuberculosis and Other Diseases, as Conducted in Eastern Europe and Central Asia Countries,” Int. J. Environ. Res. Public Heal. 2022, Vol. 19, Page 8706, vol. 19, no. 14, p. 8706, Jul. 2022, doi: 10.3390/IJERPH19148706.
A. Bennett, A. L. V. Avanceña, J. Wegbreit, C. Cotter, K. Roberts, and R. Gosling, “Engaging the private sector in malaria surveillance: a review of strategies and recommendations for elimination settings,” Malar. J. 2017 161, vol. 16, no. 1, pp. 1–19, Jun. 2017, doi: 10.1186/S12936-017-1901-1.
A. Shekar P, H. Patel, A. Dumra, D. Reddy, K. S. Shivakumar, and P. Satish Kumar, “Presentation, management and outcomes of pediatric urogenital tuberculosis: 20 years’ experience from a tertiary center,” J. Pediatr. Urol., vol. 17, no. 4, pp. 546.e1-546.e8, Aug. 2021, doi: 10.1016/j.jpurol.2021.04.002.
D. G. Storla, S. Yimer, and G. A. Bjune, “A systematic review of delay in the diagnosis and treatment of tuberculosis,” BMC Public Health, vol. 8, no. 1, pp. 1–9, Jan. 2008, doi: 10.1186/1471-2458-8-15/COMMENTS.
M. R. Sarwar and A. Saqib, “Cancer prevalence, incidence and mortality rates in Pakistan in 2012,” Cogent Med., vol. 4, no. 1, p. 1288773, Jan. 2017, doi: 10.1080/2331205X.2017.1288773.
K. Lönnroth et al., “Towards tuberculosis elimination: an action framework for low-incidence countries,” Eur. Respir. J., vol. 45, no. 4, pp. 928–952, Apr. 2015, doi: 10.1183/09031936.00214014.
C. Mukhopadhyay, T. Shaw, G. M. Varghese, and D. A. B. Dance, “Melioidosis in South Asia (India, Nepal, Pakistan, Bhutan and Afghanistan),” Trop. Med. Infect. Dis. 2018, Vol. 3, Page 51, vol. 3, no. 2, p. 51, May 2018, doi: 10.3390/TROPICALMED3020051.
W. S. Stevens, L. Scott, L. Noble, N. Gous, and K. Dheda, “Impact of the GeneXpert MTB/RIF Technology on Tuberculosis Control,” Tuberc. Tuber. Bacillus Second Ed., pp. 389–410, Sep. 2017, doi: 10.1128/9781555819569.CH18.
J. Chakaya et al., “Global Tuberculosis Report 2020 – Reflections on the Global TB burden, treatment and prevention efforts,” Int. J. Infect. Dis., vol. 113, pp. S7–S12, Dec. 2021, doi: 10.1016/j.ijid.2021.02.107.
I. A. Rana, S. S. Bhatti, and S. e Saqib, “The spatial and temporal dynamics of infrastructure development disparity – From assessment to analyses,” Cities, vol. 63, pp. 20–32, Mar. 2017, doi: 10.1016/J.CITIES.2016.12.020.
M. Irfan, Y. Hao, M. Ikram, H. Wu, R. Akram, and A. Rauf, “Assessment of the public acceptance and utilization of renewable energy in Pakistan,” Sustain. Prod. Consum., vol. 27, pp. 312–324, Jul. 2021, doi: 10.1016/J.SPC.2020.10.031.
M. W. Gondal, “URBANIZATION IN PAKISTAN AND CHALLENGES TO SOCIAL DEVELOPMENT,” Univ. PUNJAB, 2021.
A. Siddiqa, “The New Frontiers: Militancy & Radicalism in Punjab,” 2013.
A. Mahmood, A. Mahmood, R. N. Malik, and Z. K. Shinwari, “Indigenous knowledge of medicinal plants from Gujranwala district, Pakistan,” J. Ethnopharmacol., vol. 148, no. 2, pp. 714–723, Jul. 2013, doi: 10.1016/J.JEP.2013.05.035.
S. S. Hasan, Z. U. Mustafa, C. S. Kow, and H. A. Merchant, “‘Sehat Sahulat Program’: A Leap into the Universal Health Coverage in Pakistan,” Int. J. Environ. Res. Public Heal. 2022, Vol. 19, Page 6998, vol. 19, no. 12, p. 6998, Jun. 2022, doi: 10.3390/IJERPH19126998.
“Educational status and awareness among tuberculosis patients of Karachi - PubMed.” Accessed: Jun. 24, 2024. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/26968274/
M. Miandad, F. Burke, S. Nawaz-Ul-Huda, and M. Azam, “Geodemographic analysis of tuberculosis patients in Karachi, Pakistan,” Hum. Geogr., vol. 9, no. 2, pp. 165–182, Nov. 2015, doi: 10.5719/HGEO.2015.92.4.
M. Y. Mangi, Z. Yue, S. Kalwar, and Z. A. Lashari, “Comparative Analysis of Urban Development Trends of Beijing and Karachi Metropolitan Areas,” Sustain. 2020, Vol. 12, Page 451, vol. 12, no. 2, p. 451, Jan. 2020, doi: 10.3390/SU12020451.
O. Wegelin et al., “Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique?,” Eur. Urol., vol. 71, no. 4, pp. 517–531, Apr. 2017, doi: 10.1016/J.EURURO.2016.07.041.
Bagcchi, S. (2023). WHO's global tuberculosis report 2022. The Lancet Microbe, 4(1), e20. Mıandad, M., Anwar, M. M., Ahmed, S., Rahman, G., & Khan, M. A. (2019). Assessment of risk factors associated with spread of tuberculosis in Gujrat city Pakistan. Coğrafya Dergisi(39), 41-60.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 50SEA

This work is licensed under a Creative Commons Attribution 4.0 International License.