Development of a Generative AI Application for Therapy of Speech-Impaired Patients
Keywords:
Gen AI, Speech Therapy, Large Language ModelsAbstract
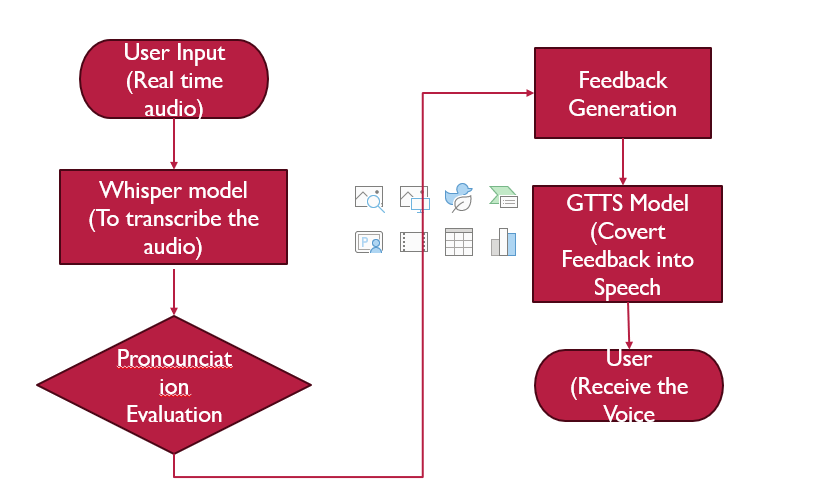
With the use of this web application, speech therapy can be provided to individuals with speech disabilities through an easy-to-use and engaging interface, which allows them to receive treatment from anywhere. Conventional treatment often requires the patient's presence, which can be hard due to their location, finances, or even other health conditions. The application helps users practice articulation, fluency, and pronunciation with the help of guided exercises, visual aids, and voice recognition technology. Users are provided with a personalized treatment plan that reviews their progress over time and provides them with feedback, reports, and reminders to help ensure users are motivated and consistent. This new technology will increase the availability of services to patients in underserved regions, which will improve their communication as well as the quality of life.
References
L. Mortensen, A. S. Meyer, and G. W. Humphreys, “Age-related effects on speech production: A review,” Lang. Cogn. Process., vol. 21, no. 1–3, pp. 238–290, Jan. 2006, doi: 10.1080/01690960444000278;JOURNAL:JOURNAL:PLCP20;WGROUP:STRING:PUBLICATION.
D. Hirtz, D. J. Thurman, K. Gwinn-Hardy, M. Mohamed, A. R. Chaudhuri, and R. Zalutsky, “How common are the ‘common’ neurologic disorders?,” Neurology, vol. 68, no. 5, pp. 326–337, Jan. 2007, doi: 10.1212/01.WNL.0000252807.38124.A3;PAGE:STRING:ARTICLE/CHAPTER.
K. S. Regina Jokel, Luc De Nil, “Speech disfluencies in adults with neurogenic stuttering associated with stroke and traumatic brain injury,” J. Med. Speech. Lang. Pathol., vol. 15, no. 3, pp. 243–261, 2007, [Online]. Available: https://www.researchgate.net/publication/279587929_Speech_disfluencies_in_adults_with_neurogenic_stuttering_associated_with_stroke_and_traumatic_brain_injury#:~:text=The six features of neurogenic,positions%3B 4) the speaker does
D. Ward, “Stuttering and cluttering: Frameworks for understanding and treatment,” Psychol. Press, 2006, [Online]. Available: https://psycnet.apa.org/record/2006-20272-000
P. van L. Aravind Kumar Namasivayam, Deirdre Coleman, Aisling O’Dwyer, “Speech Sound Disorders in Children: An Articulatory Phonology Perspective,” Front. Psychol., vol. 10, 2019, doi: https://doi.org/10.3389/fpsyg.2019.02998.
S. T. Benjamas Prathanee, Panida Thanawirattananit, “Speech, language, voice, resonance and hearing disorders in patients with cleft lip and palate,” J Med Assoc Thai, vol. 96, 2013, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/24386745/
J. R. Duffy, “Chapter 33 - Functional speech disorders: clinical manifestations, diagnosis, and management,” Handb. Clin. Neurol., vol. 139, pp. 379–388, 2016, doi: https://doi.org/10.1016/B978-0-12-801772-2.00033-3.
F. Brosseau-Lapré and S. Rvachew, “Introduction to speech sound disorders,” Plur. Publ., p. 295, 2020.
R. S. Apurba Das, Nawed Alam Bhattacharjee, Akash Pal, Dipti, “Speech and Language Disorder: Assessment and Intervention Approaches,” Int. J. Soc. Impact, vol. 9, no. 1, 2024, doi: 10.25215/2455/0901013.
A. L. Holland, “When is Aphasia Aphasia? The Problem of Closed Head Injury,” Aphasiology Arch., 1982, [Online]. Available: https://aphasiology.pitt.edu/746/
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 50sea

This work is licensed under a Creative Commons Attribution 4.0 International License.