Comprehensive Review on Postoperative Central Nervous System Infections (PCNSI): Causes, Prevention Strategies, and Therapeutic Approaches using Computer Based Electronic Health Record (EHR)
Keywords:
Craniotomy Infections, Bacterial Pathogens, Antibiotic Resistance, Cranioplasty, HER, Electronic dataAbstract
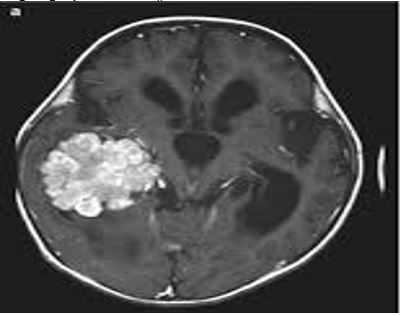
The central nervous system is susceptible to various infections. Over centuries, bacterial infections have proven lethal in various surgical procedures. Infections that occur after craniotomy are often due to the reopening of operating wounds and past contamination of the scalp. Electronic health record (EHR) although provides programs to support surveillance efforts for these infections. But the problem with these tools traditionally used is lack of accuracy. Till now, the EHR systems are giving data to monitor and plan for these infections but this system definitely needs more accuracy. The rate of postoperative infection in craniotomy ranges from 0.8% to 7% in patients who have received preoperative antibiotic prophylaxis. This rate increases significantly to about 10% in patients without antibiotic prophylaxis. Different types of bacteria manifest infections at different intervals after surgery. For instance, Streptococcus pyogenes infections typically appear within one or two days, Staphylococcal infections usually become evident after four to five days post-surgery, while gram-negative bacillary problems may arise within six or seven days. Resistance in bacteria contributes to the prevalence of postoperative infections, with examples such as Vancomycin Resistant Streptococcus aureus (VRSA), Vancomycin Resistant Enterococci (VRE), and Methicillin-Resistant Streptococcus aureus (MRSA). Given the high incidence of postoperative neurosurgical infections, there is a pressing need to manage such infections meticulously to reduce the risk of infections and associated fatalities. Treatment options include antibiotics and surgical practices aimed at minimizing pathogenic infections. Early and prompt recognition of bacterial infections after craniotomy is crucial, necessitating an understanding of both local and general infection symptoms. Additionally, cranioplasty can be considered as a means to address postoperative neurosurgical pathogenic infections.
References
I. Shah, M. A. Shaikh, and K. Mehmood, “Characteristics of Post-Neurosurgical Nosocomial Bacterial Meningitis in Adults: a retrospective Cross-Sectional Study,” Pakistan J. Med. Heal. Sci., vol. 16, no. 11, pp. 397–397, Nov. 2022, doi: 10.53350/PJMHS20221611397.
E. Journal et al., “Antibiotic therapy by intrathecal or intraventricular approach for postsurgical meningitis or ventriculitis: a systematic review and meta-analysis,” Egypt. J. Neurosurg. 2023 381, vol. 38, no. 1, pp. 1–11, May 2023, doi: 10.1186/S41984-023-00199-9.
K. Hussein, R. Bitterman, B. Shofty, M. Paul, and A. Neuberger, “Management of post-neurosurgical meningitis: narrative review,” Clin. Microbiol. Infect., vol. 23, no. 9, pp. 621–628, Sep. 2017, doi: 10.1016/j.cmi.2017.05.013.
R. N. Sahu, R. Kumar, and A. Mahapatra, “Central nervous system infection in the pediatric population,” J. Pediatr. Neurosci., vol. 4, no. SUPPL. 1, pp. 20–24, Jan. 2009, doi: 10.4103/1817-1745.49102.
Y. F. Ma, L. Wen, and Y. Zhu, “Prospective study evaluating post-operative central nervous system infections following cranial surgery,” Br. J. Neurosurg., vol. 33, no. 1, pp. 80–83, Jan. 2019, doi: 10.1080/02688697.2018.1519112.
W. Liang, Z. Yuan-Run, and Y. Min, “Clinical Presentations and Outcomes of Post-Operative Central Nervous System Infection Caused by Multi-Drug–Resistant/Extensively Drug-Resistant Acinetobacter baumannii: A Retrospective Study,” https://home.liebertpub.com/sur, vol. 20, no. 6, pp. 460–464, Aug. 2019, doi: 10.1089/SUR.2018.286.
Y. J. Shi, G. H. Zheng, L. Y. Qian, R. A. Qsman, G. G. Li, and G. J. Zhang, “
Longitudinal Analysis of Risk Factors for Clinical Outcomes of Enterobacteriaceae Meningitis/Encephalitis in Post-Neurosurgical Patients: A Comparative Cohort Study During 2014–2019
,” Infect. Drug Resist., vol. 13, pp. 2161–2170, Jul. 2020, doi: 10.2147/IDR.S252331.“Craniotomy - Wikipedia.” Accessed: Jul. 23, 2024. [Online]. Available: https://en.wikipedia.org/wiki/Craniotomy
R. Zhan et al., “Post-operative central nervous system infections after cranial surgery in China: Incidence, causative agents, and risk factors in 1,470 patients,” Eur. J. Clin. Microbiol. Infect. Dis., vol. 33, no. 5, pp. 861–866, Dec. 2014, doi: 10.1007/S10096-013-2026-2/METRICS.
J. Wen et al., “Hypothalamus-Pituitary Dysfunction as an Independent Risk Factor for Postoperative Central Nervous System Infections in Patients With Sellar Region Tumors,” Front. Endocrinol. (Lausanne)., vol. 12, p. 661305, Apr. 2021, doi: 10.3389/FENDO.2021.661305/BIBTEX.
E. Jiménez-Martínez et al., “Risk factors for surgical site infection after craniotomy: A prospective cohort study,” Antimicrob. Resist. Infect. Control, vol. 8, no. 1, pp. 1–8, May 2019, doi: 10.1186/S13756-019-0525-3/TABLES/4.
L. Cheng et al., “Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery,” Diagnostics 2023, Vol. 13, Page 2207, vol. 13, no. 13, p. 2207, Jun. 2023, doi: 10.3390/DIAGNOSTICS13132207.
N. Cassir et al., “Risk factors for surgical site infections after neurosurgery: A focus on the postoperative period,” Am. J. Infect. Control, vol. 43, no. 12, pp. 1288–1291, Dec. 2015, doi: 10.1016/j.ajic.2015.07.005.
S. M. Klimkiewicz et al., “Influence of the Built Environment on Airflow, Contamination, and Infection in the Operating Room: A Systematic Literature Review,” medRxiv, p. 2022.07.20.22277856, Jul. 2022, doi: 10.1101/2022.07.20.22277856.
V. Pintado et al., “Staphylococcus aureus meningitis in adults: A comparative cohort study of infections caused by meticillin-resistant and meticillin-susceptible strains,” J. Hosp. Infect., vol. 102, no. 1, pp. 108–115, May 2019, doi: 10.1016/j.jhin.2018.11.008.
Archana et al., “Isolation and Characterization of Lytic Bacteriophage against Methicillin Resistant Staphylococcus aureus from Pyoderma in Dog,” Indian J. Anim. Res., vol. 56, no. 7, pp. 873–879, Jul. 2022, doi: 10.18805/IJAR.B-4869.
L. Prozan, N. Popovits, Z. Lidar, and R. Ben-Ami, “Risk Factors and Outcomes of Cutibacterium acnes Postoperative Central Nervous System Infection: A Case–Control Study,” World Neurosurg., vol. 137, pp. e251–e256, May 2020, doi: 10.1016/J.WNEU.2020.01.161.
R. A. Borchardt and D. Tzizik, “Update on surgical site infections: The new CDC guidelines,” J. Am. Acad. Physician Assist., vol. 31, no. 4, pp. 52–54, Apr. 2018, doi: 10.1097/01.JAA.0000531052.82007.42.
M. A. Smith and N. R. Dahlen, “Clinical practice guideline surgical site infection prevention,” Orthop. Nurs., vol. 32, no. 5, pp. 242–248, Sep. 2013, doi: 10.1097/NOR.0B013E3182A39C6B.
P. M. Spielmann, R. Yu, and M. Neeff, “Skull base osteomyelitis: current microbiology and management,” J. Laryngol. Otol., vol. 127, no. S1, pp. S8–S12, Jan. 2013, doi: 10.1017/S0022215112002356.
H. Zhou and X. Zhang, “Intracranial malignant lesions correlate with the requirement for a long treatment course in postoperative central nervous system infection,” Neuropsychiatr. Dis. Treat., vol. 10, pp. 2071–2077, Nov. 2014, doi: 10.2147/NDT.S71836.
“(PDF) Preventing Surgical Complications During Microscopic Fenestration in Middle Fossa Arachnoid Cysts: A Retrospective Study for 38 Cases and Literature Review.” Accessed: Jul. 06, 2024. [Online]. Available: https://www.researchgate.net/publication/354138379_Preventing_Surgical_Complications_During_Microscopic_Fenestration_in_Middle_Fossa_Arachnoid_Cysts_A_Retrospective_Study_for_38_Cases_and_Literature_Review
M. Liu et al., “A retrospective study of prevalence and antibiotic resistance of bacteria isolated from the cerebrospinal fluid of neurosurgical patients in a Shanghai tertiary hospital,” Feb. 2020, doi: 10.21203/RS.2.23500/V1.
I. Martin-Loeches, A. Blake, and D. Collins, “Severe infections in neurocritical care,” Curr. Opin. Crit. Care, vol. 27, no. 2, pp. 131–138, Apr. 2021, doi: 10.1097/MCC.0000000000000796.
H. D. Mollman and S. J. Haines, “Risk factors for postoperative neurosurgical wound infection: A case-control study,” J. Neurosurg., vol. 64, no. 6, pp. 902–906, Jun. 1986, doi: 10.3171/JNS.1986.64.6.0902.
S. McClelland and W. A. Hall, “Postoperative central nervous system infection: Incidence and associated factors in 2111 neurosurgical procedures,” Clin. Infect. Dis., vol. 45, no. 1, pp. 55–59, Jul. 2007, doi: 10.1086/518580/2/45-1-55-TBL002.GIF.
W. Ma, C. Li, and L. Cong, “Dynamic Curve Analysis of Indicators Related to Lumbar Cistern Drainage for Postoperative Meningitis,” World Neurosurg., vol. 151, pp. e299–e307, Jul. 2021, doi: 10.1016/J.WNEU.2021.04.031.
T. A. M. Radwan, R. S. Fahmy, and B. N. Hanna, “Surveillance of the incidence and causative pathogens of meningitis and surgical site infection after craniotomies for brain tumors in neurosugical ICU and ward: a cohort study,” Ain-Shams J. Anesthesiol. 2018 101, vol. 10, no. 1, pp. 1–7, Oct. 2018, doi: 10.1186/S42077-018-0010-X.
K. Singh, S. Lohiya, R. Chaudhary, M. Lakra, and S. Damke, “A Rare Case of Guillain-Barré Syndrome with Signs of Meningeal Irritation and Treatment-Related Fluctuations/Relapse,” J. Pediatr. Neurol., vol. 21, no. 6, pp. 434–436, Jan. 2022, doi: 10.1055/S-0042-1750790/ID/JR2200005-16/BIB.
C. Moon, Y. G. Kwak, B. N. Kim, E. S. Kim, and C. S. Lee, “Implications of postneurosurgical meningitis caused by carbapenem-resistant Acinetobacter baumannii,” J. Infect. Chemother., vol. 19, no. 5, pp. 916–919, Jan. 2013, doi: 10.1007/s10156-013-0608-7.
J. B. Chang et al., “Combined Strategy for Post-Operative Patients with Central Nervous System Infections Caused by Extensively Drug-Resistant/Pan-Drug–Resistant Acinetobacter baumannii: A Retrospective Study,” https://home.liebertpub.com/sur, vol. 21, no. 10, pp. 853–858, Nov. 2020, doi: 10.1089/SUR.2019.341.
R. Moorthy, V. Job, G. Rebekah, and V. Rajshekhar, “Cerebrospinal Fluid Procalcitonin - A Potential Biomarker for Post-Craniotomy Bacterial Meningitis,” Neurol. India, vol. 70, no. 2, pp. 721–725, Mar. 2022, doi: 10.4103/0028-3886.344643.
R. N. Montalvo et al., “Variations in the Organisms Causing Deep Surgical Site Infections in Fracture Patients at a Level i Trauma Center (2006-2015),” J. Orthop. Trauma, vol. 32, no. 12, pp. E475–E481, 2018, doi: 10.1097/BOT.0000000000001305.
C. Mayslich, P. A. Grange, and N. Dupin, “Cutibacterium acnes as an Opportunistic Pathogen: An Update of Its Virulence-Associated Factors,” Microorg. 2021, Vol. 9, Page 303, vol. 9, no. 2, p. 303, Feb. 2021, doi: 10.3390/MICROORGANISMS9020303.
L. Zhu et al., “The Diagnostic and Antibiotic Reference Values of Procalcitonin for Intracranial Infection After Craniotomy,” World Neurosurg., vol. 126, pp. e1–e7, Jun. 2019, doi: 10.1016/J.WNEU.2018.10.241.
R. E. Balch, “Wound Infections Complicating Neurosurgical Procedures,” J. Neurosurg., vol. 26, no. 1part1, pp. 41–45, Jan. 1967, doi: 10.3171/JNS.1967.26.1PART1.0041.
J. W. Alexander, J. S. Solomkin, and M. J. Edwards, “Updated recommendations for control of surgical site infections,” Ann. Surg., vol. 253, no. 6, pp. 1082–1093, Jun. 2011, doi: 10.1097/SLA.0B013E31821175F8.
K. Y. Yang, W. N. Chang, J. T. Ho, H. C. Wang, and C. H. Lu, “Postneurosurgical nosocomial bacterial brain abscess in adults,” Infection, vol. 34, no. 5, pp. 247–251, Oct. 2006, doi: 10.1007/S15010-006-5607-5/METRICS.
N. Lange et al., “Clinical Characteristics and Course of Postoperative Brain Abscess,” World Neurosurg., vol. 120, pp. e675–e683, Dec. 2018, doi: 10.1016/J.WNEU.2018.08.143.
T. Niu, X. Bao, J. Wei, Y. Shi, W. Ma, and R. Wang, “Impact of Penicillin Allergy–Based Alternative Antibiotics on the Risk of Postoperative Central Nervous System Infection: A Retrospective Cohort Study,” World Neurosurg., vol. 171, pp. e745–e751, Mar. 2023, doi: 10.1016/J.WNEU.2022.12.102.
R. M. Antonello and N. Riccardi, “How we deal with Staphylococcus aureus (MSSA, MRSA) central nervous system infections,” Front. Biosci. - Sch., vol. 14, no. 1, p. 1, Jan. 2022, doi: 10.31083/J.FBS1401001/1945-0524-14-1-001.PDF.
M. Weller et al., “Diagnosis and management of complications from the treatment of primary central nervous system tumors in adults,” Neuro. Oncol., vol. 25, no. 7, pp. 1200–1224, Jul. 2023, doi: 10.1093/NEUONC/NOAD038.
J. M. Lemée, M. V. Corniola, M. Da Broi, K. Schaller, and T. R. Meling, “Early Postoperative Complications in Meningioma: Predictive Factors and Impact on Outcome,” World Neurosurg., vol. 128, pp. e851–e858, Aug. 2019, doi: 10.1016/J.WNEU.2019.05.010.
M. Meschiari et al., “Ceftazidime/avibactam and ceftolozane/tazobactam for the treatment of extensively drug-resistant Pseudomonas aeruginosa post-neurosurgical infections: three cases and a review of the literature,” Infection, vol. 49, no. 3, pp. 549–553, Jun. 2021, doi: 10.1007/S15010-020-01539-9/TABLES/1.
E. R. Bader, A. J. Kobets, A. Ammar, and J. T. Goodrich, “Factors predicting complications following cranioplasty,” J. Cranio-Maxillofacial Surg., vol. 50, no. 2, pp. 134–139, Feb. 2022, doi: 10.1016/J.JCMS.2021.08.001.
A. Soriano, Y. Carmeli, A. S. Omrani, L. S. P. Moore, M. Tawadrous, and P. Irani, “Ceftazidime-Avibactam for the Treatment of Serious Gram-Negative Infections with Limited Treatment Options: A Systematic Literature Review,” Infect. Dis. Ther., vol. 10, no. 4, pp. 1989–2034, Dec. 2021, doi: 10.1007/S40121-021-00507-6/TABLES/6.
G. L. Daikos et al., “Review of Ceftazidime-Avibactam for the Treatment of Infections Caused by Pseudomonas aeruginosa,” Antibiot. 2021, Vol. 10, Page 1126, vol. 10, no. 9, p. 1126, Sep. 2021, doi: 10.3390/ANTIBIOTICS10091126.
N. Rattanachak et al., “High-Throughput Transcriptomic Profiling Reveals the Inhibitory Effect of Hydroquinine on Virulence Factors in Pseudomonas aeruginosa,” Antibiotics, vol. 11, no. 10, p. 1436, Oct. 2022, doi: 10.3390/ANTIBIOTICS11101436/S1.
F. Ciummo, P. Srinivas, and J. Biedny, “Antimicrobial use in central nervous system infections,” Curr. Opin. Infect. Dis., vol. 34, no. 3, pp. 255–263, Jun. 2021, doi: 10.1097/QCO.0000000000000721.
R. Nau, F. Sörgel, and H. Eiffert, “Central nervous system infections and antimicrobial resistance: an evolving challenge,” Curr. Opin. Neurol., vol. 34, no. 3, pp. 456–467, Jun. 2021, doi: 10.1097/WCO.0000000000000931.
G. G. Zhanel et al., “Real-life experience with ceftolozane/tazobactam in Canada: results from the CLEAR (Canadian LEadership on Antimicrobial Real-life usage) registry,” J. Glob. Antimicrob. Resist., vol. 25, pp. 346–350, Jun. 2021, doi: 10.1016/J.JGAR.2021.03.025.
S. Dubler et al., “Off-Label Use of Ceftolozane/Tazobactam for the Successful Treatment of Healthcare-Associated Meningitis Caused by Extensively Drug-Resistant Pseudomonas aeruginosa in a Polytraumatized Patient—A Case Report,” Reports 2022, Vol. 5, Page 33, vol. 5, no. 3, p. 33, Aug. 2022, doi: 10.3390/REPORTS5030033.
W. Baharoon, J. Shamou, and L. Layqah, “A Fatal Case of Meningitis Complicating Chronic Otitis Media and Base of Skull Osteomyelitis due to Carbapenemase (OXA-48)-Producing Klebsiella pneumoniae,” Dr. Sulaiman Al Habib Med. J. 2022 51, vol. 5, no. 1, pp. 23–28, Dec. 2022, doi: 10.1007/S44229-022-00024-9.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 50SEA

This work is licensed under a Creative Commons Attribution 4.0 International License.