Analyzing the Predictors of Mortality Among Asphyxiated Neonates
Keywords:
Mortality, Neonates, Asphyxia, PredictorsAbstract
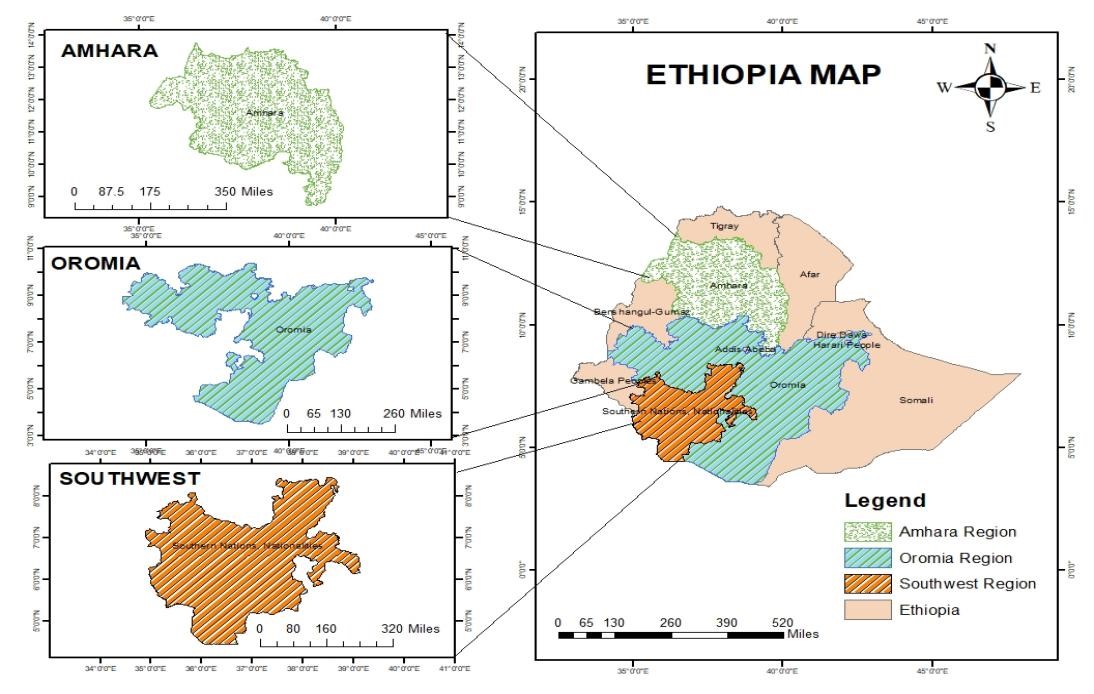
Birth asphyxia refers to the inability to initiate and sustain breathing at birth, leading to inadequate oxygen supply to vital organs. It is one of the most common causes of perinatal brain injury, contributing to high rates of morbidity and mortality. Neonatal asphyxia is a major cause of early neonatal death, accounting for an estimated 900,000 deaths annually. It results from impaired respiratory gas exchange in the fetus or newborn, causing hypoxia, hypercapnia, and, in some cases, ischemia. This condition can affect multiple organs, leading to biochemical and functional changes, such as lactic acidosis, which may result in death or severe neurological impairment. Neonatal asphyxia is frequently associated with multiple organ failure, primarily impacting the brain, heart, and kidneys. It can lead to complications affecting motor, sensory, cognitive, and psychological development. Several factors contribute to birth asphyxia, including maternal anemia, diabetes, and placental abruption. Other significant predictors of mortality among asphyxiated neonates include neonatal sepsis, preterm birth, lack of Kangaroo Mother Care (KMC), low birth weight, seizures, need for resuscitation at birth, stage III asphyxia, hypoxic-ischemic encephalopathy (stages II and III), seizures and thrombocytopenia. This systematic review aims to identify the pooled predictors of mortality among asphyxiated neonates. Various online databases, including PubMed, MEDLINE, Google Scholar, and WHO websites, were searched for relevant studies. The review included cross-sectional, case-control, and cohort studies conducted in Pakistan and Ethiopia. Data entry and statistical analysis were performed using Excel and SPSS (version 27). The pooled mortality rate of birth asphyxia was found to be 64.0%. Among asphyxiated neonates, 27.1% who were delivered via spontaneous vaginal delivery (SVD) did not survive. Mortality rates were 39.4% for neonates born after prolonged labor, 42.6% for those delivered following premature rupture of membranes, and 50% for those weighing less than 2500g at birth. Additionally, 60.2% of asphyxiated neonates with seizures and 35.7% requiring resuscitation at birth did not survive. The highest mortality rate (81.1%) was observed in neonates with stage III asphyxia. It is concluded that asphyxiated neonates exhibit a high mortality rate. Key predictors of mortality include neonatal sepsis, vaginal delivery, lack of Kangaroo Mother Care (KMC), low birth weight, seizures, need for resuscitation at birth, stage III asphyxia, advanced maternal age, delivery complications, and prolonged rupture of membranes.
References
F. M. A. Daniel Bekele Ketema, “Birth Asphyxia Related Mortality in Northwest Ethiopia: A Multi-Centre Cohort Study,” PLoS One, vol. 18, no. 2, p. 2, 2023, [Online]. Available: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0281656
A. R. Farhana Tabassum, “Risk Factors Associated with Birth Asphyxia in Rural District Matiari, Pakistan: A Case Control Study,” Int. J. Clin. Med., vol. 5, no. 21, 2014, [Online]. Available: https://www.scirp.org/journal/paperinformation?paperid=52796
E. Y. R. et al. Gemechu Gelan Bekele, “Incidence and Predictors of Mortality Among Neonates admitted with Birth asphyxia to neonatal intensive care unit of West Shewa Zone Public Hospitals, Central Ethiopia,” BMJ Paediatr. Open, 2024, [Online]. Available: https://bmjpaedsopen.bmj.com/content/8/1/e002403
S. M. R. Syed Bilal Hassan, “Risk Factors Associated with Birth Asphyxia: A Case Control Study,” Ann. King Edward Med. Univ., 2021, [Online]. Available: https://www.annalskemu.org/journal/index.php/annals/article/view/4883
H. G. Muhammad Haris, “Neonatal Blood Gases and Outcomes Following Perinatal Asphyxia,” Pak-Euro J. Med. Life Sci 7, Spec., vol. 2, no. 12, 2024, [Online]. Available: https://readersinsight.net/PJMLS/article/view/3198
S. A. G. Sana Noor, Kousar Praveen, Muhammad Hussain, Muhammad Afzal, “Observational Study on Standard Practices of Nurses in Birth Asphaxia Management at a Tertiary Care Hospital, Lahore, Pakistan,” Natl. J. Heal. Sci., vol. 5, pp. 24–29, 2020, [Online]. Available: https://njhsciences.com/wp-content/uploads/2020/07/Article4F.pdf
E. B. W. Muluken Amare Wudu, “Incidence and Predictors of Mortality Among Neonates Admitted with Birth Asphyxia to Neonatal intensive Care units in Ethiopia: a Systematic Review and Meta-analysis,” BMC Pediatr., 2025, [Online]. Available: https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-025-05481-3
M. F. Tegegne YS, Birhan TY, Takele H, “Incidence and development of validated mortality prediction model among asphyxiated neonates admitted to neonatal intensive care unit at Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, Northwest Ethiopia, 2021: retrospective follow-up study,” BMC Pediatr., vol. 24, no. 1, 2024, doi: 10.1186/s12887-024-04696-0.
I. A. Memon, “Acute kidney injury in neonates with birth asphyxia at a tertiary care hospital,” Pakistan J. Med. Heal. Sci., pp. 573–575, 2021, [Online]. Available: https://pjmhsonline.com/2021/march/573.pdf
M. U. K. Javaria Younus, Sikandar Hayat, Farah Haroon, Khawaja Ahmad Irfan Waheed, Mazhar Qadir Khan, “Correlation Of Severity Of Metabolic Acidosis At Admission And Outcome In Asphyxiated Neonates,” J Ayub Med Coll Abbottabad, vol. 32, no. 2, 2020, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/32583992/
H. M. A.-H. Muhammad Amin, Muhammad Saleem, Shamas-un- Nisa, Malik Muhammad Naeem, “BIRTH ASPHYXIA; SHORT-TERM OUTCOME OF NEONATES TREATED WITH ALLOPURINOL,” Prof. Med. J., vol. 24, no. 6, 2017, [Online]. Available: https://theprofesional.com/index.php/tpmj/article/view/1214
S. Z. Lyaba Atta, Hamid Naeem, Subhanullah Syed, “Frequency of Acute Kidney Injury among Neonates with Birth Asphyxia Presenting at Tertiary Care Hospital in Khyber Pakhtunkhwa,” Pakistan J. Heal. Sci., 2024, [Online]. Available: https://www.thejas.com.pk/index.php/pjhs/article/view/1987
T. B. T. et al Belete Fenta Kebede, “Time to death and predictors of mortality among asphyxiated neonates in southwest Ethiopia, 2022: prospective cohort study,” BMJ J., vol. 14, no. 1, p. 1, 2024, [Online]. Available: https://bmjopen.bmj.com/content/14/1/e077943
G. K. Lencho Kajela solbana, Solomon Berhanu, Yenealem Gezahegn, “Survival Status and Predictors of Mortality Among Asphyxiated Neonates Admitted to Jimma University Medical Center, Southwest Ethiopia: A Retrospective Cohort Study,” Heal. Sci. Reports, vol. 8, no. 2, p. 2, 2025, [Online]. Available: https://onlinelibrary.wiley.com/doi/10.1002/hsr2.70482
Rubeena Parveen Dhiloo, “Maternal Risk Factors for Birth Asphyxia in Low-Resource Communities,” J. Soc. Obstet. Gynaecol. Pakistan, vol. 14, no. 1, 2024, [Online]. Available: http://jsogp.net/index.php/jsogp/article/view/757
T. G. A. & B. T. Dawit Tesfaye Daka, Chalachew Adugna Wubneh, “Incidence and predictors of Mortality Among Neonates Admitted with Perinatal Asphyxia at west Oromia tertiary hospitals, Ethiopia, 2022,” BMC Pediatr., 2023, [Online]. Available: https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-023-04313-6
M. A. R. Noreen Samad, Samia Farooq, Kinza Hafeez, Mukharma Maryam, “Analysis of Consequences of Birth Asphyxia in Infants: A Regional Study in Southern Punjab, Pakistan,” J Coll Physicians Surg Pak, vol. 26, no. 12, 2016, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/28043304/
Z. M. Y. Yibeltal Asmamaw Yitayew, “Survival status and predictors of mortality among asphyxiated neonates admitted to the NICU of Dessie Comprehensive Specialized Hospital, Amhara Region, Northeast Ethiopia,” Plosone, 2022, [Online]. Available: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0279451
A. R. Ghazanfar Nadeem, “Risk Factors Associated With Birth Asphyxia in Term Newborns at a Tertiary Care Hospital of Multan, Pakistan,” Cureus, vol. 13, no. 10, p. 10, 2021, [Online]. Available: https://www.cureus.com/articles/73547-risk-factors-associated-with-Birth-Asphyxia-in-term-Newborns-at-a-Tertiary-Care-Hospital-Of-Multan-Pakistan#!/
T. M. D. & Z. A. G. Sisay Girma Yehouala, Esubalew Tesfahun, “Time to recovery of Asphyxiated Neonates and its’ Predictors Among Newborns Admitted to Neonatal intensive care unit at Debre Berhan Comprehensive Specialized Hospital, Ethiopia,” BMC Public Health, 2024, [Online]. Available: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-19520-8
S. T. Muhammad Asif Siddiqui, Sehrish Masood, Tayyaba Butt, “Neonatal Outcomes of Birth Asphyxia in Tertiary Care Hospital of low-income Country,” J. Fatima Jinnah Med. Univ., vol. 15, no. 1, pp. 23–26, 2021, doi: 10.37018/unkh2664.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 50sea

This work is licensed under a Creative Commons Attribution 4.0 International License.