Maximum Value Attribute based Decision Tree and Random Forest for COVID-19 Prediction
Keywords:
COVID-19 Prediction, MVA, Symptoms, Rough Set TheoryAbstract
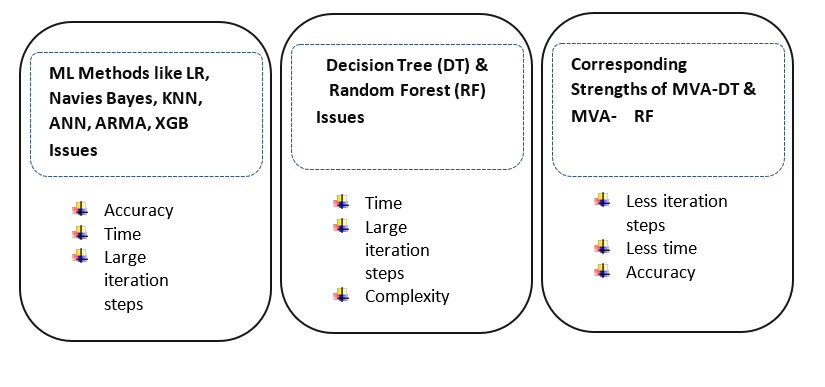
The COVID-19 pandemic emerged as one of the most disruptive global health crises of the century, affecting social and economic systems worldwide. The rapid rise in infections placed immense pressure on healthcare infrastructures, demanding fast and reliable diagnostic tools. In recent years, Machine Learning (ML) has gained considerable importance in the medical field, supporting the diagnosis of conditions such as heart failure, pneumonia, dengue, breast cancer, and diabetes. In a similar way, clinical symptoms related to COVID-19 can be utilized to support early prediction, helping limit transmission. Although ensemble learning techniques such as Decision Trees and Random Forests have shown strong predictive performance for COVID-19, they often require more time and a larger number of iterations, which can be challenging when rapid detection is needed.
This study focuses on improving the efficiency of COVID-19 prediction by integrating Rough Set Theory (RST) through the Maximum Value Attribute (MVA) approach with classical Decision Tree (DT) and Random Forest (RF) models. The objective is to reduce computation time and iterations while maintaining reliable diagnostic accuracy. The proposed method classifies patients as COVID-19 positive or negative based on eight key clinical symptoms. A dataset containing clinical records of 136,294 patients, collected from an open-source GitHub repository, was used for evaluation. Four models—DT, RF, MVA-DT, and MVA-RF—were implemented in Python using Jupyter Notebook. Standard evaluation metrics were applied to assess performance. Overall, the MVA-DT model achieved the most efficient execution, while the MVA-RF model demonstrated strong predictive capability with an accuracy of 95.82%, precision of 81.90%, recall of 59.28%, and an F1 score of 68.77%.
References
D. P. Kavadi, R. Patan, M. Ramachandran, and A. H. Gandomi, “Partial derivative Nonlinear Global Pandemic Machine Learning prediction of COVID 19,” Chaos, Solitons & Fractals, vol. 139, p. 110056, Oct. 2020, doi: 10.1016/J.CHAOS.2020.110056.
A. Khakharia et al., “Outbreak Prediction of COVID-19 for Dense and Populated Countries Using Machine Learning,” Ann. Data Sci. 2020 81, vol. 8, no. 1, pp. 1–19, Oct. 2020, doi: 10.1007/S40745-020-00314-9.
A. A. Alrajhi et al., “Data-Driven Prediction for COVID-19 Severity in Hospitalized Patients,” Int. J. Environ. Res. Public Heal. 2022, Vol. 19, Page 2958, vol. 19, no. 5, p. 2958, Mar. 2022, doi: 10.3390/IJERPH19052958.
L. J. Muhammad, E. A. Algehyne, S. S. Usman, A. Ahmad, C. Chakraborty, and I. A. Mohammed, “Supervised Machine Learning Models for Prediction of COVID-19 Infection using Epidemiology Dataset,” SN Comput. Sci. 2020 21, vol. 2, no. 1, pp. 11-, Nov. 2020, doi: 10.1007/S42979-020-00394-7.
J. Uddin, R. Ghazali, M. M. Deris, U. Iqbal, and I. A. Shoukat, “A novel rough value set categorical clustering technique for supplier base management,” Comput. 2021 1039, vol. 103, no. 9, pp. 2061–2091, Apr. 2021, doi: 10.1007/S00607-021-00950-W.
Y. Zoabi, S. Deri-Rozov, and N. Shomron, “Machine learning-based prediction of COVID-19 diagnosis based on symptoms,” npj Digit. Med. 2021 41, vol. 4, no. 1, pp. 3-, Jan. 2021, doi: 10.1038/s41746-020-00372-6.
Y. Zoabi and N. Shomron, “COVID-19 diagnosis prediction by symptoms of tested individuals: a machine learning approach,” medRxiv, p. 2020.05.07.20093948, May 2020, doi: 10.1101/2020.05.07.20093948.
S. Subudhi et al., “Comparing machine learning algorithms for predicting ICU admission and mortality in COVID-19,” npj Digit. Med. 2021 41, vol. 4, no. 1, pp. 87-, May 2021, doi: 10.1038/s41746-021-00456-x.
N. Shakhovska, V. Yakovyna, V. Chopyak, N. Shakhovska, V. Yakovyna, and V. Chopyak, “A new hybrid ensemble machine-learning model for severity risk assessment and post-COVID prediction system,” Math. Biosci. Eng. 2022 66102, vol. 19, no. 6, pp. 6102–6123, 2022, doi: 10.3934/MBE.2022285.
D. K. Sharma, M. Subramanian, P. Malyadri, B. S. Reddy, M. Sharma, and M. Tahreem, “Classification of COVID-19 by using supervised optimized machine learning technique,” Mater. Today Proc., vol. 56, pp. 2058–2062, Jan. 2022, doi: 10.1016/J.MATPR.2021.11.388.
H. Coppock, A. Gaskell, P. Tzirakis, A. Baird, L. Jones, and B. Schuller, “End-to-end convolutional neural network enables COVID-19 detection from breath and cough audio: a pilot study,” BMJ Innov., vol. 7, no. 2, pp. 356–362, Apr. 2021, doi: 10.1136/BMJINNOV-2021-000668.
P. Patwa et al., “Can Self Reported Symptoms Predict Daily COVID-19 Cases?,” May 2021, Accessed: Dec. 09, 2025. [Online]. Available: https://arxiv.org/pdf/2105.08321
Z. Li et al., “Efficient management strategy of COVID-19 patients based on cluster analysis and clinical decision tree classification,” Sci. Reports 2021 111, vol. 11, no. 1, pp. 9626-, May 2021, doi: 10.1038/s41598-021-89187-3.
R. K. Mojjada, A. Yadav, A. V. Prabhu, and Y. Natarajan, “WITHDRAWN: Machine learning models for covid-19 future forecasting,” Mater. Today Proc., Dec. 2020, doi: 10.1016/J.MATPR.2020.10.962.
E. Fayyoumi, S. Idwan, and H. Aboshindi, “Machine Learning and Statistical Modelling for Prediction of Novel COVID-19 Patients Case Study: Jordan,” Int. J. Adv. Comput. Sci. Appl., vol. 11, no. 5, pp. 122–126, May 2020, doi: 10.14569/IJACSA.2020.0110518.
Y. Gao et al., “Machine learning based early warning system enables accurate mortality risk prediction for COVID-19,” Nat. Commun. 2020 111, vol. 11, no. 1, pp. 5033-, Oct. 2020, doi: 10.1038/s41467-020-18684-2.
A. H. M. Hassan, A. A. M. Qasem, W. F. M. Abdalla, and O. H. Elhassan, “Visualization & Prediction of COVID-19 Future Outbreak by Using Machine Learning,” Int. J. Inf. Technol. Comput. Sci., vol. 13, no. 3, pp. 16–32, Jun. 2021, doi: 10.5815/IJITCS.2021.03.02.
A. Alotaibi, M. Shiblee, and A. Alshahrani, “Prediction of Severity of COVID-19-Infected Patients Using Machine Learning Techniques,” Comput. 2021, Vol. 10, Page 31, vol. 10, no. 3, p. 31, Mar. 2021, doi: 10.3390/COMPUTERS10030031.
S. T. Ogunjo, I. A. Fuwape, and A. B. Rabiu, “Predicting COVID‐19 Cases From Atmospheric Parameters Using Machine Learning Approach,” GeoHealth, vol. 6, no. 4, p. e2021GH000509, Apr. 2022, doi: 10.1029/2021GH000509.
V. K. Gupta, A. Gupta, D. Kumar, and A. Sardana, “Prediction of COVID-19 confirmed, death, and cured cases in India using random forest model,” Big Data Min. Anal., vol. 4, no. 2, pp. 116–123, Jun. 2021, doi: 10.26599/BDMA.2020.9020016.
N. Rochmawati et al., “Covid Symptom Severity Using Decision Tree,” Proceeding - 2020 3rd Int. Conf. Vocat. Educ. Electr. Eng. Strength. Framew. Soc. 5.0 through Innov. Educ. Electr. Eng. Informatics Eng. ICVEE 2020, Oct. 2020, doi: 10.1109/ICVEE50212.2020.9243246.
M. H. Tayarani N., “Applications of artificial intelligence in battling against covid-19: A literature review,” Chaos, Solitons & Fractals, vol. 142, p. 110338, Jan. 2021, doi: 10.1016/j.chaos.2020.110338.
S. Roy and P. Ghosh, “Factors affecting COVID-19 infected and death rates inform lockdown-related policymaking,” PLoS One, vol. 15, no. 10, p. e0241165, Oct. 2020, doi: 10.1371/JOURNAL.PONE.0241165.
K. B. Prakash, “Analysis, Prediction and Evaluation of COVID-19 Datasets using Machine Learning Algorithms,” Int. J. Emerg. Trends Eng. Res., vol. 8, no. 5, pp. 2199–2204, May 2020, doi: 10.30534/IJETER/2020/117852020.
H. R. Niazkar and M. Niazkar, “Application of artificial neural networks to predict the COVID-19 outbreak,” Glob. Heal. Res. Policy 2020 51, vol. 5, no. 1, pp. 50-, Nov. 2020, doi: 10.1186/S41256-020-00175-Y.
X. Guan et al., “Clinical and inflammatory features based machine learning model for fatal risk prediction of hospitalized COVID-19 patients: results from a retrospective cohort study,” Ann. Med., vol. 53, no. 1, pp. 257–266, 2021, doi: 10.1080/07853890.2020.1868564;ISSUE:ISSUE:DOI.
D. Darwin, D. Christian, W. Chandra, and M. Nababan, “Comparison of Decision Tree and Linear Regression Algorithms in the Case of Spread Prediction of COVID-19 in Indonesia,” J. Comput. Networks, Archit. High Perform. Comput., vol. 4, no. 1, pp. 1–12, Jan. 2022, doi: 10.47709/CNAHPC.V4I1.1234.
M. S. Satu et al., “Short-Term Prediction of COVID-19 Cases Using Machine Learning Models,” Appl. Sci. 2021, Vol. 11, Page 4266, vol. 11, no. 9, p. 4266, May 2021, doi: 10.3390/APP11094266.
D. Chumachenko, I. Meniailov, K. Bazilevych, T. Chumachenko, and S. Yakovlev, “Investigation of Statistical Machine Learning Models for COVID-19 Epidemic Process Simulation: Random Forest, K-Nearest Neighbors, Gradient Boosting,” Comput. 2022, Vol. 10, Page 86, vol. 10, no. 6, p. 86, May 2022, doi: 10.3390/COMPUTATION10060086.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 50sea

This work is licensed under a Creative Commons Attribution 4.0 International License.