Prediction of Elective Patients and Length of Stay in Hospital
Keywords:
Hospital Management, Patient Stay Duration, Patient Location, Machine Learning AlgorithmsAbstract
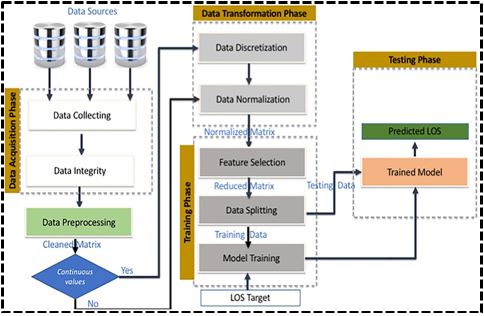
The efficient management of hospital resources and the optimization of patient care are critical tasks in healthcare systems worldwide. One of the key challenges in hospital management is predicting the duration of a patient's stay and accurately determining their location within the hospital, such as whether they are in the Intensive Care Unit (ICU) or the Operating Theater (OT). In this study, we address this problem statement by employing machine learning algorithms to predict both the stay duration and the location of patients within the hospital. The methods applied in this study include Random Forest, Support Vector Machine (SVM), and K-nearest neighbors (KNN) algorithms. These algorithms utilize patient demographic information such as age, weight, and severity of disease as features to predict the stay duration and location. The dataset used for this study consists of a revised dataset containing relevant patient information. Upon applying the machine learning algorithms, we obtained promising results. The Random Forest algorithm achieved the highest accuracy of 88.6% in predicting patient locations, followed by SVM with an accuracy of 60.8% and KNN with an accuracy of 58.1%. Additionally, Random Forest exhibited superior precision, recall, and F1-scores for both ICU and OT classifications compared to SVM and KNN. The results obtained from this study have several practical implications and potential uses. Firstly, accurate predictions of patient stay duration and location can aid hospital administrators in resource allocation and planning, enabling them to efficiently manage bed occupancy and staffing levels. Additionally, healthcare providers can use these predictions to anticipate patient needs and allocate resources accordingly, thereby enhancing patient care and satisfaction. Moreover, the machine learning algorithms utilized in this study can be integrated into hospital information systems to automate the prediction process, providing real-time insights to healthcare professionals. In conclusion, the application of machine learning algorithms in predicting patient stay duration and location within the hospital offers promising results and valuable insights for hospital management. By leveraging patient demographic information and advanced predictive models, healthcare institutions can improve operational efficiency, enhance patient care delivery, and ultimately optimize resource utilization.
References
D. A. Huntley, D. W. Cho, J. Christman, and J. G. Csernansky, “Predicting length of stay in an acute psychiatric hospital,” Psychiatr. Serv., vol. 49, no. 8, pp. 1049–1053, Aug. 1998, doi: 10.1176/PS.49.8.1049/ASSET/IMAGES/LARGE/B511T4.JPEG.
A. Lim and P. Tongkumchum, “Methods for Analyzing Hospital Length of Stay with Application to Inpatients Dying in Southern Thailand,” Glob. J. Health Sci., vol. 1, no. 1, p. p27, Mar. 2009, doi: 10.5539/GJHS.V1N1P27.
K. C. Chang, M. C. Tseng, H. H. Weng, Y. H. Lin, C. W. Liou, and T. Y. Tan, “Prediction of Length of Stay of First-Ever Ischemic Stroke,” Stroke, vol. 33, no. 11, pp. 2670–2674, Nov. 2002, doi: 10.1161/01.STR.0000034396.68980.39.
S. Shea, R. V. Sideli, W. Dumouchel, G. Pulver, R. R. Arons, and P. D. Clayton, “Computer-generated Informational Messages Directed to Physicians: Effect on Length of Hospital Stay,” J. Am. Med. Informatics Assoc., vol. 2, no. 1, pp. 58–64, Jan. 1995, doi: 10.1136/JAMIA.1995.95202549.
V. J. Wheatley and J. I. Baker, “‘Please, I want to go home’: ethical issues raised when considering the choice of place of care in palliative care,” Postgrad. Med. J., vol. 83, no. 984, pp. 643–648, Oct. 2007, doi: 10.1136/PGMJ.2007.058487.
T. L. Rodziewicz and J. E. Hipskind, “Medical error prevention,” StatPearls [Internet]. StatPearls Publ., 2019.
F. M. Simmons, “CEU: Hospital overcrowding: An opportunity for case managers,” Case Manager, vol. 16, no. 4, pp. 52–54, Jul. 2005, doi: 10.1016/J.CASEMGR.2005.06.004.
A. Scott, A. Shiell, and M. G. Farnworth, “The value of early discharge: Dispelling some myths,” Health Policy (New. York)., vol. 26, no. 2, pp. 81–91, Dec. 1993, doi: 10.1016/0168-8510(93)90111-2.
A. Clarke, “Why are we trying to reduce the length of stay? Evaluation of the costs and benefits of reducing time in hospital must start from the objectives that govern change.,” BMJ Qual. Saf., vol. 5, no. 3, pp. 172–179, Sep. 1996, doi: 10.1136/QSHC.5.3.172.
D. Moher et al., “Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement,” PLoS Med., vol. 6, no. 7, Jul. 2009, doi: 10.1371/JOURNAL.PMED.1000097.
J. A. Hayden, D. A. van der Windt, J. L. Cartwright, P. Côté, and C. Bombardier, “Assessing bias in studies of prognostic factors,” Ann. Intern. Med., vol. 158, no. 4, pp. 280–286, Feb. 2013, doi: 10.7326/0003-4819-158-4-201302190-00009/SUPPL_FILE/AIME201302190-00009_SUPPL1.XLSX.
M. Bauer, L. Fitzgerald, E. Haesler, and M. Manfrin, “Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence,” J. Clin. Nurs., vol. 18, no. 18, pp. 2539–2546, Sep. 2009, doi: 10.1111/J.1365-2702.2008.02685.X.
M. S. Ullah, H. Qayoom, and F. Hassan, “Viral Pneumonia Detection Using Modified GoogleNet Through Lung X-rays,” 2021 4th Int. Symp. Adv. Electr. Commun. Technol. ISAECT 2021, 2021, doi: 10.1109/ISAECT53699.2021.9668553.
P. Yoon, I. Steiner, and G. Reinhardt, “Analysis of factors influencing length of stay in the emergency department,” Can. J. Emerg. Med., vol. 5, no. 3, pp. 155–161, 2003, doi: 10.1017/S1481803500006539.
J. E. Mezzich and G. A. Coffman, “Factors Influencing Length of Hospital Stay,” https://doi.org/10.1176/ps.36.12.1262, vol. 36, no. 12, Apr. 2006, doi: 10.1176/PS.36.12.1262.
C. S. Yang, C. P. Wei, C. C. Yuan, and J. Y. Schoung, “Predicting the length of hospital stay of burn patients: Comparisons of prediction accuracy among different clinical stages,” Decis. Support Syst., vol. 50, no. 1, pp. 325–335, Dec. 2010, doi: 10.1016/J.DSS.2010.09.001.
R. Stoean, C. Stoean, A. Sandita, D. Ciobanu, and C. Mesina, “Ensemble of Classifiers for Length of Stay Prediction in Colorectal Cancer,” Lect. Notes Comput. Sci. (including Subser. Lect. Notes Artif. Intell. Lect. Notes Bioinformatics), vol. 9094, pp. 444–457, 2015, doi: 10.1007/978-3-319-19258-1_37.
B. Shickel, P. J. Tighe, A. Bihorac, and P. Rashidi, “Deep EHR: A Survey of Recent Advances in Deep Learning Techniques for Electronic Health Record (EHR) Analysis,” IEEE J. Biomed. Heal. Informatics, vol. 22, no. 5, pp. 1589–1604, Sep. 2018, doi: 10.1109/JBHI.2017.2767063.
P. Yadav, M. Steinbach, V. Kumar, and G. Simon, “Mining electronic health records (EHRs): A survey,” ACM Comput. Surv., vol. 50, no. 6, Jan. 2018, doi: 10.1145/3127881/SUPPL_FILE/YADAV.ZIP.
A. Rajkomar et al., “Scalable and accurate deep learning with electronic health records,” npj Digit. Med. 2018 11, vol. 1, no. 1, pp. 1–10, May 2018, doi: 10.1038/s41746-018-0029-1.
H. Harutyunyan, H. Khachatrian, D. C. Kale, G. Ver Steeg, and A. Galstyan, “Multitask learning and benchmarking with clinical time series data,” Sci. Data 2019 61, vol. 6, no. 1, pp. 1–18, Mar. 2017, doi: 10.1038/s41597-019-0103-9.
G. Qadir, S. Zareen, F. Hassan, and A. U. Rahman, “Voice Spoofing Countermeasure Based on Spectral Features to Detect Synthetic Attacks Through LSTM,” Int. J. Innov. Sci. Technol., vol. 3, no. 4, pp. 153–165, 2021, Accessed: Jun. 24, 2024. [Online]. Available: https://journal.50sea.com/index.php/IJIST/article/view/124
A. Awad, M. Bader–El–Den, and J. McNicholas, “Patient length of stay and mortality prediction: A survey,” http://dx.doi.org/10.1177/0951484817696212, vol. 30, no. 2, pp. 105–120, Mar. 2017, doi: 10.1177/0951484817696212.
“Melanoma Detection Using a Deep Learning Approach | International Journal of Innovations in Science & Technology.” Accessed: Jun. 24, 2024. [Online]. Available: https://journal.50sea.com/index.php/IJIST/article/view/191
“Modelling for the Planning and Management of Bed Capacities in Hospitals on JSTOR.” Accessed: Jun. 24, 2024. [Online]. Available: https://www.jstor.org/stable/822874
P. R. Harper, “A framework for operational modelling of hospital resources,” Health Care Manag. Sci., vol. 5, no. 3, pp. 165–173, 2002, doi: 10.1023/A:1019767900627/METRICS.
A. X. Costa, S. A. Ridley, A. K. Shahani, P. R. Harper, V. De Senna, and M. S. Nielsen, “Mathematical modelling and simulation for planning critical care capacity*,” Anaesthesia, vol. 58, no. 4, pp. 320–327, Apr. 2003, doi: 10.1046/J.1365-2044.2003.03042.X.
K. Godfrey, “Compartmental models and their application”, [Online]. Available: https://tauruspet.med.yale.edu/staff/edm42/courses/ENAS_915_2013/book-chapters/Godfrey_ch2.pdf
P. H. Millard, “Geriatric medicine: a new method of measuring bed usage and a theory for planning, MD Thesis St,” Georg. Hosp. Med. Sch. Univ. London, 1988.
G. W. Harrison and P. H. Millard, “Balancing acute and long-term care: The mathematics of throughput in departments of geriatric medicine,” Methods Inf. Med., vol. 30, no. 3, pp. 221–228, 1991, doi: 10.1055/S-0038-1634832/ID/BR1634832-13/BIB.
H. G.W., “Compartmental models of hospital patient occupancy patterns. Modelling hospital resource use: a different approach to the planning and control of health care systems,” R. Soc. Med., pp. 53–61, 1994.
M. D. Mackay, M., Lee, “Using Compartmental Models to Predict Hospital Bed Occupancy,” Dep. Psychol. Univ. Adelaide, pp. 1–18, 2007.
S. I. Millard, P. H., McClean, “Go with the flow: a systems approach to healthcare planning,” (Royal Soc. Med. Press Limited, London), 1996.
J. A. García-Navarro and W. A. Thompson, “Analysis of bed usage and occupancy following the introduction of geriatric rehabilitative care in a hospital in Huesca, Spain,” Health Care Manag. Sci., vol. 4, no. 1, pp. 63–66, 2001, doi: 10.1023/A:1009657817365/METRICS.
A. Banjar, H. Dawood, A. Javed, and F. Hassan, “Fall event detection using the mean absolute deviated local ternary patterns and BiLSTM,” Appl. Acoust., vol. 192, p. 108725, Apr. 2022, doi: 10.1016/J.APACOUST.2022.108725.
F. Hassan, S. Albahli, A. Javed, and A. Irtaza, “A Robust Framework for Epidemic Analysis, Prediction and Detection of COVID-19,” Front. Public Heal., vol. 10, p. 805086, May 2022, doi: 10.3389/FPUBH.2022.805086/BIBTEX.
E. Ei-Darzi, C. Vasilakis, T. J. Chaussalet, and P. H. Millard, “A Simulation Model to Evaluate the Interaction between Acute, Rehabilitation, Long Stay Care and the Community,” pp. 475–485, 2000, doi: 10.1007/978-1-4757-4919-9_31.
C. Vasilakis and E. El-Darzi, “A simulation study of the winter bed crisis,” Health Care Manag. Sci., vol. 4, no. 1, pp. 31–36, 2001, doi: 10.1023/A:1009649615548/METRICS.
R. Davies and H. Davies, “Modelling patient flows and resource provision in health systems,” Omega, vol. 22, no. 2, pp. 123–131, Mar. 1994, doi: 10.1016/0305-0483(94)90073-6.
“Comparative Analysis of Machine Learning Algorithms for Classification of Environmental Sounds and Fall Detection | International Journal of Innovations in Science & Technology.” Accessed: Jun. 24, 2024. [Online]. Available: https://journal.50sea.com/index.php/IJIST/article/view/188
S. I. McClean, B. McAlea, and P. H. Millard, “Using a markov reward model to estimate spend- down costs for a geriatric department,” J. Oper. Res. Soc., vol. 49, no. 10, pp. 1021–1025, Sep. 1998, doi: 10.1057/PALGRAVE.JORS.2600619/METRICS.
G. Kimberly Sabsay (LSI, “Learning from our past: Using medical history to guide patient care”, [Online]. Available: https://insights.princeton.edu/2021/01/analytics-patient-care/
M. P. Taylor G., McClean S., “Continuous-time Markov models for geriatric patient behaviour,” Appl. Stoch. Model. Bus. Ind., vol. 13, no. (3-4), pp. 315–323, 1997.
Taylor, G., McClean, S.I., Millard, P.H., “A model to analyse the flow of elderly patients around departments of geriatric medicine and the community. Go with the Flow: A Systems Approach to Healthcare Planning,” 1996.
G. J. Taylor, S. I. McClean, and P. H. Millard, “Stochastic Models of Geriatric Patient Bed Occupancy Behaviour,” J. R. Stat. Soc. Ser. A Stat. Soc., vol. 163, no. 1, pp. 39–48, Jan. 2000, doi: 10.1111/1467-985X.00155.
“Decision Trees for Classification: A Machine Learning Algorithm”, [Online]. Available: https://www.xoriant.com/blog/decision-trees-for-classification-a-machine-learning-algorithm#:~:text=Introduction Decision Trees are a,namely decision nodes and leaves.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 50SEA

This work is licensed under a Creative Commons Attribution 4.0 International License.