Real Time Detection of Diabetic Retinopathy using Deep Learning Techniques
Keywords:
Diabetic Retinopathy, Diabetes Mellitus, VGG16, ResNet50, Custom CNN ModelAbstract
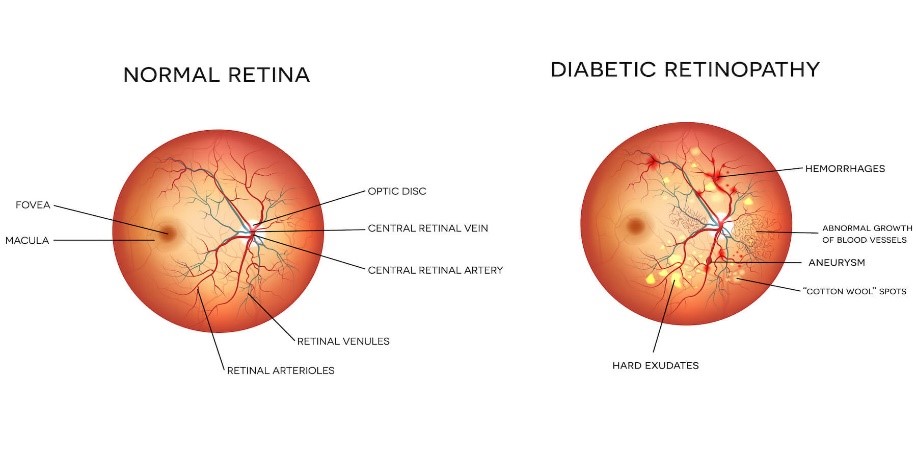
Diabetic Retinopathy is a prevalence disease which is a medical condition frequently caused due to high sugar levels of blood. It deteriorates the optic nerve as it compresses and blurs the vision, which is used to detect white light and transmits signals to your cerebrum using a nerve. There has been a massive increase in the statistics having diabetic retinopathy which causes the loss of sight in any age group with no treatment Every diabetic patient is required to visit their ophthalmologist after every two weeks or mandatorily in a month. Moreover, bi-annual inspection is required to notice the amount of vision to see the objects. For this reason, Pakistan lacks to have ophthalmologist which are expert in their domain. Mostly, they are not available round the clock especially in less privileged areas. Therefore, we have developed a smartphone-based handheld AI-integrated product which is cost-effective and portable which detects the visual Impairment and produces reports of the concern patient with a minor intervention on the same day by an eye specialist. This research project focuses on diabetic retinopathy detection by utilizing 20D (20 Diopter) Lens and camera of any random smart phone which captures fundus images which are further spitted and compared against various models of deep learning . In this research, VGG-15, ResNet50 and Custom CNN was undertaken. As a result, VGG16 outperformed other models by obtaining highest validation accuracy that is 74.53% as well as lowest validation loss of 55.94%. Moreover, ResNet50 yielded 74.08% validation accuracy and computing validation loss of 58.72%. Consequently, Custom CNN Model achieves 57.26% validation accuracy and 57.26% validation loss. Thus, VGG16 performed best on the dataset provided and is deployed in the smartphone application which is a portable and cost-effective method for Diabetic Retinopathy screening in less privileged areas. This project aims to target three Sustainable Development Goals including Affordable and clean energy ,Good health and well-being, and Industry Innovation and Infrastructure respectively.
References
Y. Kang, Y. Fang, and X. Lai, “Automatic Detection of Diabetic Retinopathy with Statistical Method and Bayesian Classifier,” J. Med. Imaging Heal. Informatics, vol. 10, no. 5, pp. 1225–1233, Feb. 2020, doi: 10.1166/JMIHI.2020.3025.
M. Ashraf, P. L. Nesper, L. M. Jampol, F. Yu, and A. A. Fawzi, “Statistical Model of Optical Coherence Tomography Angiography Parameters That Correlate With Severity of Diabetic Retinopathy,” Invest. Ophthalmol. Vis. Sci., vol. 59, no. 10, pp. 4292–4298, Aug. 2018, doi: 10.1167/IOVS.18-24142.
C. H. Tan, B. M. Kyaw, H. Smith, C. S. Tan, and L. T. Car, “Use of smartphones to detect diabetic retinopathy: Scoping review and meta-analysis of diagnostic test accuracy studies,” J. Med. Internet Res., vol. 22, no. 5, 2020, doi: 10.2196/16658.
G. U. Parthasharathi, K. Vasantha Kumar, R. Premnivas, and K. Jasmine, “Diabetic Retinopathy Detection Using Machine Learning,” J. Innov. Image Process., vol. 4, no. 1, pp. 26–33, May 2022, doi: 10.36548/JIIP.2022.1.003.
S. Stolte and R. Fang, “A survey on medical image analysis in diabetic retinopathy,” Med. Image Anal., vol. 64, p. 101742, 2020, doi: 10.1016/j.media.2020.101742.
W. L. Alyoubi, W. M. Shalash, and M. F. Abulkhair, “Diabetic retinopathy detection through deep learning techniques: A review,” Informatics Med. Unlocked, vol. 20, p. 100377, Jan. 2020, doi: 10.1016/J.IMU.2020.100377.
R. E. Hacisoftaoglu, M. Karakaya, and A. B. Sallam, “Deep learning frameworks for diabetic retinopathy detection with smartphone-based retinal imaging systems,” Pattern Recognit. Lett., vol. 135, pp. 409–417, Jul. 2020, doi: 10.1016/J.PATREC.2020.04.009.
I. Odeh, M. Alkasassbeh, and M. Alauthman, “Diabetic Retinopathy Detection using Ensemble Machine Learning,” 2021 Int. Conf. Inf. Technol. ICIT 2021 - Proc., pp. 173–178, Jul. 2021, doi: 10.1109/ICIT52682.2021.9491645.
R. Rajalakshmi, V. Prathiba, S. Arulmalar, and M. Usha, “Review of retinal cameras for global coverage of diabetic retinopathy screening,” Eye 2020 351, vol. 35, no. 1, pp. 162–172, Nov. 2020, doi: 10.1038/s41433-020-01262-7.
T. Spencer, J. A. Olson, K. C. McHardy, P. F. Sharp, and J. V. Forrester, “An image-processing strategy for the segmentation and quantification of microaneurysms in fluorescein angiograms of the ocular fundus,” Comput. Biomed. Res., vol. 29, no. 4, pp. 284–302, 1996, doi: 10.1006/cbmr.1996.0021.
A. Soni and A. Rai, “A Novel Approach for the Early Recognition of Diabetic Retinopathy using Machine Learning,” 2021 Int. Conf. Comput. Commun. Informatics, ICCCI 2021, 2021, doi: 10.1109/ICCCI50826.2021.9402566.
X. Zhang et al., “Exudate detection in color retinal images for mass screening of diabetic retinopathy,” Med. Image Anal., vol. 18, no. 7, pp. 1026–1043, 2014, doi: 10.1016/j.media.2014.05.004.
L. Tang, M. Niemeijer, J. M. Reinhardt, M. K. Garvin, and M. D. Abramoff, “Splat feature classification with application to retinal hemorrhage detection in fundus images,” IEEE Trans. Med. Imaging, vol. 32, no. 2, pp. 364–375, 2013, doi: 10.1109/TMI.2012.2227119.
R. A. Welikala et al., “Automated detection of proliferative diabetic retinopathy using a modified line operator and dual classification,” Comput. Methods Programs Biomed., vol. 114, no. 3, pp. 247–261, May 2014, doi: 10.1016/J.CMPB.2014.02.010.
K. A. Goatman, A. D. Fleming, S. Philip, G. J. Williams, J. A. Olson, and P. F. Sharp, “Detection of new vessels on the optic disc using retinal photographs,” IEEE Trans. Med. Imaging, vol. 30, no. 4, pp. 972–979, Apr. 2011, doi: 10.1109/TMI.2010.2099236.
E. Treatment and D. Retinopathy, “Grading Diabetic Retinopathy from Stereoscopic Color Fundus Photographs—An Extension of the Modified Airlie House Classification: ETDRS Report Number 10,” Ophthalmology, vol. 98, no. 5, pp. 786–806, 1991, doi: 10.1016/S0161-6420(13)38012-9.
W. Zhang et al., “Automated identification and grading system of diabetic retinopathy using deep neural networks,” Knowledge-Based Syst., vol. 175, pp. 12–25, 2019, doi: 10.1016/j.knosys.2019.03.016.
K. M. Adal, P. G. Van Etten, J. P. Martinez, K. W. Rouwen, K. A. Vermeer, and L. J. Van Vliet, “An automated system for the detection and classification of retinal changes due to red lesions in longitudinal fundus images,” IEEE Trans. Biomed. Eng., vol. 65, no. 6, pp. 1382–1390, 2018, doi: 10.1109/TBME.2017.2752701.
M. Niemeijer, M. D. Abràmoff, and B. Van Ginneken, “Information fusion for diabetic retinopathy CAD in digital color fundus photographs,” IEEE Trans. Med. Imaging, vol. 28, no. 5, pp. 775–785, 2009, doi: 10.1109/TMI.2008.2012029.
R. Casanova, S. Saldana, E. Y. Chew, R. P. Danis, C. M. Greven, and W. T. Ambrosius, “Application of Random Forests Methods to Diabetic Retinopathy Classification Analyses,” PLoS One, vol. 9, no. 6, p. e98587, Jun. 2014, doi: 10.1371/JOURNAL.PONE.0098587.
S. Sanromà, A. Moreno, A. Valls, P. Romero, S. De La Riva, and R. Sagarra, “Assessment of diabetic retinopathy risk with random forests,” ESANN 2016 - 24th Eur. Symp. Artif. Neural Networks, no. April, pp. 313–318, 2016.
A. Herliana, T. Arifin, S. Susanti, and A. B. Hikmah, “Feature Selection of Diabetic Retinopathy Disease Using Particle Swarm Optimization and Neural Network,” 2018 6th Int. Conf. Cyber IT Serv. Manag. CITSM 2018, no. Citsm, pp. 2016–2019, 2019, doi: 10.1109/CITSM.2018.8674295.
M. Memon, M. M., Jawaid, M. M., Narejo, S., & Rathi, “Computer-Assisted Framework for Automatic Detection of Structural Hand Deformities,” J. Hunan Univ. Nat. Sci., vol. 48, no. 10, 2021, Accessed: May 22, 2024. [Online]. Available: http://jonuns.com/index.php/journal/article/view/826
T. Shanthi and R. S. Sabeenian, “Modified Alexnet architecture for classification of diabetic retinopathy images,” Comput. Electr. Eng., vol. 76, pp. 56–64, Jun. 2019, doi: 10.1016/J.COMPELECENG.2019.03.004.
A. R. Wahab Sait, “A Lightweight Diabetic Retinopathy Detection Model Using a Deep-Learning Technique,” Diagnostics 2023, Vol. 13, Page 3120, vol. 13, no. 19, p. 3120, Oct. 2023, doi: 10.3390/DIAGNOSTICS13193120.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 50SEA

This work is licensed under a Creative Commons Attribution 4.0 International License.